Abstract
Most of the global population live in low-income and middle-income countries (LMICs), which have historically received a small fraction of global resources for mental health. The COVID-19 pandemic has spread rapidly in many of these countries. This Review examines the mental health implications of the COVID-19 pandemic in LMICs in four parts. First, we review the emerging literature on the impact of the pandemic on mental health, which shows high rates of psychological distress and early warning signs of an increase in mental health disorders. Second, we assess the responses in different countries, noting the swift and diverse responses to address mental health in some countries, particularly through the development of national COVID-19 response plans for mental health services, implementation of WHO guidance, and deployment of digital platforms, signifying a welcome recognition of the salience of mental health. Third, we consider the opportunity that the pandemic presents to reimagine global mental health, especially through shifting the balance of power from high-income countries to LMICs and from narrow biomedical approaches to community-oriented psychosocial perspectives, in setting priorities for interventions and research. Finally, we present a vision for the concept of building back better the mental health systems in LMICs with a focus on key strategies; notably, fully integrating mental health in plans for universal health coverage, enhancing access to psychosocial interventions through task sharing, leveraging digital technologies for various mental health tasks, eliminating coercion in mental health care, and addressing the needs of neglected populations, such as children and people with substance use disorders. Our recommendations are relevant for the mental health of populations and functioning of health systems in not only LMICs but also high-income countries impacted by the COVID-19 pandemic, with wide disparities in quality of and access to mental health care.
Introduction
Although much has been written about the mental health implications of COVID-19,1, 2 greater attention has been given to high-income countries (HICs) than to low-income and middle-income countries (LMICs), where 83% of the global population live. LMICs have historically received a small fraction of global health resources for mental health.3 Furthermore, COVID-19 is now spreading rapidly in many of these settings. The relationship between mental health and COVID-19 among the vast population of LMICs is the focus of this Review.
Major risk factors for mortality from COVID-19, such as medical comorbidities including diabetes or heart disease,4 are increasingly common in LMICs, especially among individuals with lower educational levels.5, 6 Despite the lower average age of populations in LMICs compared with that in HICs offering some potential protection, the high prevalence of comorbidities, along with generally low levels of access to universal health coverage,7 paint a worrying picture in terms of the potential for lives to be lost to the pandemic. Leaving aside the direct health effects of COVID-19, the knock-on effects of efforts to contain the pandemic, such as lockdowns, closure of schools, shifting allocation of health resources, and curtailed livelihood opportunities, have the potential to be devastating and long-lasting. These measures are particularly detrimental for poor and vulnerable people in countries with weak social safety nets and inadequate economic resources to buffer against lost livelihoods. Global economic growth is expected to contract by 5–8% during and following the pandemic, pushing up to 100 million people into extreme poverty.8
The expected vulnerability of LMICs to the negative mental health sequelae of COVID-19 can be compared with the impressive efforts in many of these resource-limited countries to develop nationwide policies to address the pandemic itself and its mental health consequences. Some LMICs have developed model programmes to address the pre-existing mental health-care needs and increasing distress related to the pandemic, and have implemented guidance on psychosocial programmes from WHO and international organisations. The sensitivity and comprehensiveness of these mental health responses in some LMICs can be a model for other countries, which are suffering from fragmented mental health responses, minimal financial investment, and scarce outreach to the most vulnerable populations.9
In this Review, we examine the global mental health implications of the COVID-19 pandemic in four parts: first, the impact of the pandemic on mental health; second, the responses in different countries; third, the opportunity that the pandemic presents to reimagine global mental health; and finally, a future vision for mental health systems. Although our concerns begin with a focus on LMICs, the pandemic has shown the profoundly interconnected nature of global health and the opportunities for experiences and knowledge to inform the mental health response in all countries.
As the COVID-19 pandemic is still unfolding at the time of writing, and much of the research on mental health concerns is ongoing, this Review seeks to provide a narrative overview of some prominent findings to date. We also attempt to look into the future to anticipate the potential longer-term mental health effects that will emerge in the aftermath of the health, economic, and social consequences of the pandemic.
The impacts of the COVID-19 pandemic on mental health
The COVID-19 pandemic has exposed the already large treatment gap in mental health across LMICs, and threatens to widen it. New demands for mental health care in these countries intersect with fragile health systems, scarce resources and workforce capacity, social unrest and violence in response to COVID-19 containment strategies, and overall scarce and inequitable access to evidence-based interventions.10, 11, 12 It can be speculated that the long-term consequences on mental health will be particularly severe in the lowest resourced and most impoverished regions of the globe, where there was virtually no access to mental health services before the pandemic.13
Immediate impacts
Emerging reports on the impacts of the COVID-19 pandemic on mental health have primarily documented the increase in symptoms of mental health distress, which might reflect a normative response to the extraordinary uncertainties and difficulties experienced by populations. For example, reports have documented increased prevalence of psychological distress among health-care staff,14, 15 associated with stigma and fear of the disease.16 That said, these reports could also imply a shifting of the population distribution of distress and a consequent increase in the prevalence of clinically significant mental health problems. This theory is congruent with the few studies on the prevalence of mental health disorders that we have identified. For example, a nationwide online study of more than 10 000 individuals in Bangladesh reported a 33% prevalence of depression and 5% prevalence of suicidal ideation.17 Thus, recognising acute stress responses is essential for preventive interventions to reduce the incidence of clinically significant conditions and to build systems that address the rising needs for mental health care.
In LMICs worldwide, population-wide distress can be attributed to continued uncertainties about the spread of the disease, the effectiveness of containment strategies, and when and how everyday life will return to some resemblance of familiarity.18 These experiences of distress are exacerbated by actions aimed at mitigating the spread of COVID-19, in which governments in many LMICs have implemented strict measures (eg, use of lockdowns). These measures and related policy decisions have had unprecedented effects on the economic and social sectors in countries where the vast majority of people are employed in the informal labour market and where threats to their livelihood are already leading to public resistance and, sometimes, violence.13, 19 For instance, use of force by law enforcement and the authorities has been reported in several countries.20, 21, 22, 23 There have been reports of violence, arrests, and the abduction of journalists and activists documenting questionable government policies, corruption, and mismanagement in response to COVID-19.20, 24, 25 The pandemic is also exposing the fact that particular vulnerable groups, such as prisoners, patients in psychiatric hospitals or social care homes, people with disabilities, or women experiencing domestic violence or abuse, might be at even greater risk of psychological distress because pre-existing failures in human rights protection are worsened,21, 26 further complicating other mental health consequences related to COVID-19.14, 15
Threats of the pandemic towards mental health can be observed by systemic social inequities across demographic (eg, age, ethnicity, caste, religion, gender), economic (eg, income, assets, unemployment), neighbourhood (eg, housing structure or overcrowding), and sociocultural (eg, social support, social capital, education) characteristics.19, 27, 28 In high-income settings, low educational levels and indices of economic and social disadvantage, such as poor or overcrowded housing and homelessness, unemployment, social isolation, and loneliness, are important risk factors for contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).29, 30 As poverty and socioeconomic inequities are prominent in LMICs, and with poor coverage of adequately resourced health-care and social safety nets, it is plausible to expect mental health problems in large sections of communities across LMICs. For example, this pattern is already apparent in Brazil where the greatest risk of disease transmission is among the poorest communities in the country.31
Older populations are among the most affected by the COVID-19 pandemic in terms of illness severity and mortality. They are also more likely to suffer psychological impacts due to isolation, which is complicated by pre-existing physical health problems and medical comorbidities, and reduced access to care.32, 33 Additionally, lockdowns and the diversion of all health-care services to COVID-19 control and care affects people living with serious mental illnesses, for whom access to mental health care has been hindered during the pandemic.34 Therefore, COVID-19 is likely to lead to the recurrence or worsening of disorders among this group, who are also more likely to have other risk factors.
Another particularly vulnerable group are front-line health workers who have been deployed and redeployed for various tasks to try to contain the pandemic.35, 36 Risk factors include settings where many health workers have inadequate personal protective equipment, experiencing stigma and discrimination because of their profession, personal fears of infecting their families and loved ones, isolation from family members, and being quarantined.37, 38 Mental health effects of the pandemic among health workers have also manifested as experiences of trauma and confusion, especially in the context of lack of clarity on how to effectively treat patients with COVID-19.39, 40, 41
Long-term impacts
Without massive global action, the COVID-19 pandemic is expected to have worldwide negative impacts on economic and other social determinants of health in the long term. Mental health conditions most susceptible to negative social determinants include anxiety, mood, and disorders related to trauma and stress, which are already leading contributors to disability worldwide, according to the Global Burden of Disease study.42 The pandemic is laying the foundations for a potential worldwide suicide increase as a result of increased exposure to known risk factors, such as economic stress, job insecurity and unemployment, social isolation, decreased access to community support, barriers to mental health treatment, and exacerbated physical health problems, especially among older adults.33, 39, 43 A model combining data from multiple countries, including both HICs and LMICs, suggests that job losses due to COVID-19 might result in up to 9570 additional suicides per year worldwide.43 Time-trend regression models following the pandemic in the USA showed a forecast of 3235 excess suicides over 2 years attributable to the economic downturn (3·3% increase per year) if the unemployment increase is moderated, and an 8164 excess suicides over 2 years (8·4% increase per year) if the increase is extreme.44
No such models currently exist for LMICs. However, given that LMICs bear the bulk of the global burden of suicide45 and are especially vulnerable to economic devastation from the pandemic, it can be speculated that suicide rates could increase markedly in these countries. This theory is supported by a review of Indian media on COVID-19 and suicide.46 One concern is that in many LMICs, suicides often go under-reported or are reported as different causes of death due to the associated stigma, as well as other cultural or religious considerations.47, 48 Therefore, it will be essential to ensure transparent and rigorous reporting and monitoring of suicides in the months and years ahead, not only to fully ascertain the impacts of the pandemic but also to identify whether there are regional differences in suicide rates and to develop responses to mitigate these risk factors. Similarly, substance use disorders represent another major cause of mortality associated with previous global recessions, leading to a rise in so-called deaths of despair in affected communities.49
Prolonged school closures are likely to have a profound effect on the mental health of children, adolescents, and young adults globally.50 Aside from the important academic benefits of schooling, schools have an essential role in shaping the mental wellbeing of young people by providing a structured and supervised space for socioemotional development, friendship and social support networks, protection from risk-taking behaviours and exploitative labour, delays to early marriage and childbearing, and gatekeeper services to detect and intervene early to reduce child abuse. Furthermore, schools often represent a key access point for food for children in many LMICs.51 School meal and feeding programmes are essential for ensuring sufficient nutrition while promoting academic performance and cognitive development.52, 53 Therefore, the school closures in response to the pandemic might have the unintended consequence of increasing food insecurity among children,54 which negatively affects mental health.
The response to mental health needs
To date, there is little evidence on the impact of mental health programmes for multiple reasons: the COVID-19 pandemic is still progressing in many countries, most programmes are being implemented under real-world public health emergency circumstances with no resources for evaluation, and there has been insufficient time since the onset of the pandemic to complete and publish comprehensive evaluations. Thus, the purpose of this section is to highlight the variety and innovativeness of programmes that have been initiated. The initiative and ability of governments in LMICs to develop COVID-19 mental health plans is in itself an important observation. Similarly, the ability to launch and implement diverse programmes addressing population-level and individual clinical needs offers lessons about implementation, even if claims about effectiveness cannot yet be made for most of these initiatives. Going forward, it will be important to evaluate implementation processes and outcomes, not least to inform the mental health response to future public health emergencies, such as the extent to which the shift of care delivery from in-person to remote addresses individual clinical needs equitably or the extent to which low-cost positive psychology approaches adequately address population mental health needs.
Population initiatives
Since the start of the pandemic, there have been growing efforts to develop international guidance, national policies, and resources for LMICs to address mental health and psychosocial support (MHPSS) needs (figure 1 ).55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74 In February, 2020, the Inter-Agency Standing Committee, which coordinates responses to humanitarian emergencies, issued one of the first briefing notes with MHPSS recommendations for COVID-19.55 The brief highlighted approaches for specific populations, such as older people, children, front-line workers, and individuals in quarantine, as well as guidance on combating stigma. Shortly after this event, the International Federation of the Red Cross and Red Crescent Societies (IFRC) called for widespread use of psychological first aid, including remote delivery to people in quarantine, health workers, and groups with previous vulnerabilities (eg, mental and substance use disorders).75 The International Organization for Migration provided guidelines for forced and labour migrants.59 The Africa Centres for Disease Control and Prevention also released guidelines on MHPSS for COVID-19.71 In May, 2020, the UN released a policy brief that synthesised and added political weight to these recommendations.70
Figure 1.
Timeline of mental health and psychosocial support guidance, policies, and resources in LMICs during the initial months of the COVID-19 pandemic
IASC=Inter-Agency Standing Committee. IFRC=International Federation of Red Cross and Red Crescent Societies. IOM=International Organization for Migration.
Many of the guidelines in response to COVID-19 were grounded in pre-COVID-19 approaches to MHPSS in humanitarian settings, and the experience of implementing MHPSS services in LMICs.76, 77, 78 Notable among these are Inter-Agency Standing Committee MHPSS guidelines published in 2007,64 which have been continually revised and supplemented with additional guidance. These guidelines are organised as a pyramid of services with four layers: basic services and security, strengthening community and family, focused non-specialised supports, and specialised services.79 Furthermore, many LMICs have gained considerable expertise in addressing MHPSS in response to humanitarian emergencies,80, 81 and there is emerging consensus on the central principles for supporting individuals in such contexts. Some of these principles include the recommendations by Hobfoll and colleagues,82 which address five domains: safety, calm, self-efficacy and community efficacy, connectedness, and hope.
Therefore, on the basis of previous humanitarian emergencies and the unique needs of the COVID-19 pandemic, many LMICs rapidly developed COVID-19 national MHPSS response plans. The National Health Commission of China developed guidelines on emergency psychological crisis intervention, emphasising that mental health services should be organised at city, municipal, and provincial levels, and included psychological outreach teams and hotlines.57 In March, 2020, Lebanon issued a government action plan for a MHPSS response, outlining mental health promotion and mitigation of COVID-19 related stressors, support for people in quarantine and front-line workers, and continuity of services for patients with pre-existing mental illness.61 Similar national action plans were released in South Africa,62 Kenya,63 Uganda,64 the Maldives,65 and India.66 Some regional responses within countries preceded national plans. For example, the Kerala State Government in India constituted a multidisciplinary team in February, 2020, which integrated efforts by several sectors and established a state helpline.83
Materials have been developed in many LMICs to promote self-help for stress management during the COVID-19 pandemic and beyond. WHO developed Doing what matters in times of stress: an illustrated guide.67 The stress management self-help techniques can be practised with just a few minutes each day and include accompanying audio exercises. Released originally in English, with other translations underway, the guide is freely available for use and adaptation, and can be offered as guided or unguided self-help. In India, Firework, a short-format, 30-second, decentralised video platform that began in 2019, launched #sparkthejoy, a social impact campaign that encourages people to do an “act of good”.84 Use of the platform doubled during the period between lockdowns in India from the beginning of March to the end of May, 2020.85 The Mental Health Innovation Network and WHO launched Stories from the field: providing mental health and psychosocial support during the COVID-19 pandemic69 to share MHPSS innovation and best practice through personal narratives from health-care workers worldwide. Information, education, and communication materials highlighting mental health and stigma have been produced by many institutions and organisations implementing or supporting responses in LMICs, such as the IFRC Reference Centre for Psychosocial Support. In China, mental health education materials were produced and disseminated through WeChat, Weibo, and TikTok.86 A series of videos on grief and mental health as part of the Regional Psychosocial Support Initiative has been developed for children and adolescents in South Africa.
Detection and care
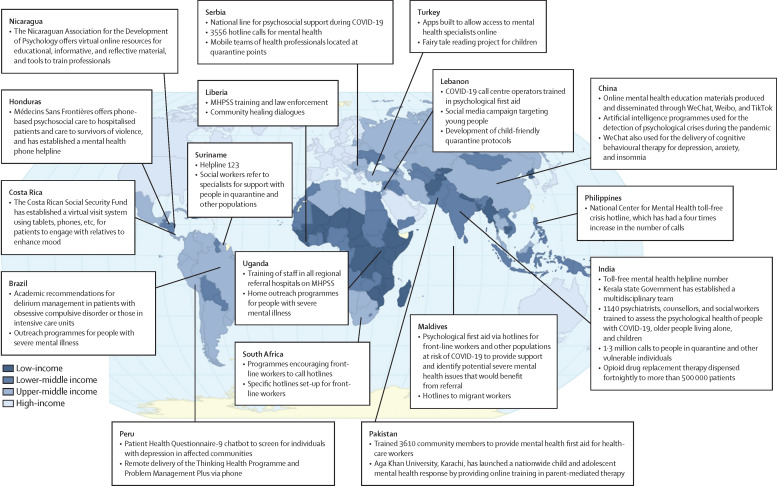
In many countries, members of the health-care system, ranging from community health workers to mental health specialists, have been trained to help detect individuals with mental illness and psychological distress (figure 2 ). Phone-based programmes in Kerala, India, and in-person initiatives in Pakistan and Uganda have been used to identify and refer people in need of care.87, 88 In China, individuals at risk of suicide can be recognised by the artificial intelligence programme Tree Holes Rescue by analysing the messaging service Weibo.57 In Peru, Socios en Salud has disseminated information via mass media to engage with a chatbot that provides free automated depression screening and referral.89
Figure 2.
Mental health responses to COVID-19 in low-income and middle-income countries
MHPSS=mental health and psychosocial support.
However, in most settings in LMICs, ongoing in-person mental health services have been disrupted and patients with severe mental illness and substance use disorders are often unable to obtain medications, attend treatment facilities, or receive social services.34 People with severe mental health conditions and intellectual disabilities, along with various other disabilities, are disproportionately likely to be in institutions, which are often not safe in relation to risk of SARS-CoV-2 infection and where care has often been compromised during the crisis.90 In some settings, outpatient services have been suspended or inpatient psychiatric facilities temporarily repurposed to treat patients with COVID-19.91 Seeking psychiatric care, especially from hospital facilities, has decreased because of concerns about SARS-CoV-2 infection and stigma due to associations of institutionalised settings with COVID-19 transmission.92 In Iran, implementation of drug use rehabilitation has been disrupted due to travel restrictions, a shift towards COVID-19 priorities,93 and rejection of external support (eg, expelling Médecins Sans Frontières94). In other settings, hospitals and drug and alcohol services have been overwhelmed with large influxes of patients facing substance use withdrawal following lockdown, with many countries suspending alcohol sales during lockdown (eg, South Africa and India). There is a debate regarding the ethics of forced abstinence.95
Face-to-face services have been maintained in parts of some LMICs, indicating considerable variability in the response of the mental health-care system.96 For example, in Punjab, India, opioid drug replacement therapy was successfully implemented.97 In Brazil, a hybrid model of in-person and remote services was instituted for individuals with psychotic disorders, including depot antipsychotic injections delivered during in-home visits, in which food insecurity was monitored.98 A similar model of home visits for patients with severe mental illness is ongoing in Uganda amid the pandemic.99
Furthermore, governments, health-care providers, and other institutions in many LMICs have adapted to the challenges imposed by physical distancing, disrupted public transportation, and lockdowns by shifting to remote services, ranging from suicide and mental health helplines, to voice-only phone-based services, to video services over smartphones or other digital devices. To help promote public mental health during the COVID-19 pandemic, the Indonesian Government, through the Ministry of Health, launched Sejiwa (ie, healthy mind) as a counselling hotline service.100 From its launch date on April 29 to May 28, 2020, Sejiwa provided 14 916 hotline consultations with a workforce of 737 volunteer psychologists from the Indonesian Psychology Association. Similar helplines have experienced heavy use in India,101, 102 Nigeria,103 the Philippines,104 and many other LMICs. Helplines have also been used for specific populations, such as south Asian labour migrants in Gulf countries and other settings.58
In the Maldives and other countries, helplines have provided psychological first aid to front-line workers.58 In South Africa, videos were developed for health-care workers highlighting symptoms of stress, anxiety, and depression, with links to seek assistance. These videos were distributed via social media. Non-governmental psychology and counselling groups in the country also offered free counselling via phone or Zoom to health-care workers during the height of the outbreak.105 In China, WeChat-based resources have been widely established throughout the country to provide free, 24 h services, including cognitive behavioural therapy.57 In the Philippines, health-care workers and repatriated overseas Filipino workers can book appointments for online or phone-based MHPSS services.104 These services predominantly address general psychological distress and common mental disorders, such as depression and anxiety, as well as suicidality.
A major initiative has been building capacities among non-specialists to deliver psychological services remotely. Problem Management Plus, a five-session psychological intervention based on problem solving therapy and designed for delivery by non-specialists in humanitarian settings,106 has been adapted for remote training and delivery (eg, voice-only phone or with video) by the IFRC in east African countries,107 Socios en Salud in Peru, and other organisations. In Peru, individuals identified to have depression with the chatbot89 are referred for remote Problem Management Plus. Another problem-solving therapy, the Friendship Bench, which is delivered by non-specialists in Zimbabwe, is now being adapted for online delivery.108 Based on the large demand for psychological services to be delivered remotely, WHO has adapted the Ensuring Quality in Psychological Support (EQUIP) platform.68 The result, EQUIP-remote, includes guidance on preparing for remote delivery (eg, confidentiality and technology issues), delivering supervision for remote services, and managing suicidality in remote delivery, as well as a competency assessment tool to support safe delivery of psychological services. These recommendations are an extension of WHO's overall guidance on assuring quality and comprehensive care in the shift from in-person to remote delivery of health services during the COVID-19 pandemic.73
However, access to these interventions is not equitably distributed. Settings with restricted phone, electricity, or WiFi access cannot engage in all of these services. People with disabilities who, as well as being exposed to other social determinants of mental ill health and exposure to COVID-19, often encounter practical barriers to accessing support, and many of the interventions delivered are often not accessible to those with sensory impairments.109 In relation to children and adolescents, mental health care that would have otherwise been delivered via school counsellors or student health services has been disrupted as a result of school and university closures.50 One innovation in Pakistan has been the launch of nationwide, free, online training sessions in parent-mediated therapy to support rehabilitative care of children with disabilities by Aga Khan University, Karachi.110
Infectious disease control efforts integrating mental health principles
A valuable lesson learned from the Ebola virus outbreak was that MHPSS services are important not only for reducing mental health problems but also for effective infectious disease control.111, 112 Initial suspicion in some communities that Ebola virus was a government conspiracy led to the realisation in west Africa that engagement with communities, families, and individuals needed to focus on trust building, listening skills, and managing distress.113 Therefore, in response to the outbreak, community healing dialogues were an important MHPSS initiative to build trust and engagement with public health recommendations for infection control.114 This response showed that MHPSS training was vital for contact tracers to build trust, support treatment engagement, and recognise distress that would benefit from mental health services.111 Thus, psychological first aid training is now recommended for contact tracers during infectious disease control.115 Currently, in Liberia, half of the 3 day training curriculum for contact tracers in the COVID-19 response is devoted to MHPSS content.
During the Ebola virus outbreak, the IFRC advocated the five-pillar response for effective disease control: community engagement or social mobilisation, surveillance and contact tracing, case management and treatment, safe and dignified burials and disinfection, and overall psychosocial support. Lessons learned from this outbreak in west Africa also highlight the need to assure the mental health and psychosocial wellbeing of health workers, which is equally important now in response to COVID-19.116 Similarly, during the Ebola virus outbreak, law enforcement personnel also benefited from MHPSS training to assist in home visits and staffing of treatment centres,117 and de-escalation training is recommended for COVID-19 first responders in Lebanon. In Lebanon, child-friendly quarantine guidelines incorporate MHPSS to increase the likelihood of successful infection control while minimising child and family distress.61Figure 3 provides an overall model of MHPSS treatment, detection, and integration in COVID-19 responses.
Figure 3.
Detection and care strategies for mental illness, and the role of mental health and psychosocial support in infectious disease control
Reimagining the principles of global mental health
The COVID-19 pandemic has disrupted many previous certainties about the way that societies are organised, and the relationship between governments and their citizens and between nations; however, it also offers a window of opportunity to rethink old assumptions and to re-evaluate priorities in and approaches to global mental health. We argue that global mental health can and must do better to successfully respond to the mental health challenges posed by COVID-19 globally. These efforts will involve hastening the shift from the treatment gap notion, with its implicit biomedical emphasis, to a broader care gap perspective,118 increased recognition of the crucial contribution of civil society and local leadership, and action beyond the health sector, to make the contexts in which people grow up, live, work, and age more promoting of mental health. Although the framework shift that we propose is not new,119 it has not yet been achieved at scale. To accomplish this goal, we set out key opportunities organised around three dimensions for change: context (ie, where), stakeholders (ie, who), and sectors (ie, what).
Context: the where of global mental health
The COVID-19 pandemic has shown that successful public health responses are not necessarily correlated with national gross domestic product. Some LMICs in Asia and Africa have shown how the pandemic can be managed with minimal loss of life, whereas some HICs in Europe and North America have had some of the highest mortality rates in the world.120 The pandemic indicates that the time has come to abandon the HIC versus LMIC dichotomy, which obscures meaningful variations within and between contexts, and too often carries an implicit assumption of unidirectional learning. Moving beyond these categories by thinking in terms of differently resourced settings, we can recognise the diversity of resources including, but not limited to, financial resources that distinguish between contexts globally and can be harnessed to face crises and improve health. For example, religious centres, community ties, family support structures, traditional healers, village leaders, and youth groups are all contextually varying resources that are essential to engage with to overcome mental and physical health threats, including those of COVID-19.121, 122, 123 Compared with deficit-based assessments of resources, typically defined in terms of money and biomedical resources, strength-based assessments provide more nuanced perspectives on the assets of heterogeneous contexts and avoid the displacement of effective local strategies by imported, context-free approaches.121 Much can be learned from implementation research methodologies that measure local conditions and evaluate context-dependent mechanisms of change when evaluating interventions and implementation strategies for mental health care across settings.125
A new architecture of global mental health is emerging, which challenges the view that LMICs are simply data collection sites126, 127 or test beds for interventions developed in HICs, and promotes equitable, mutually beneficial partnerships with HICs.99 Insights from LMICs will be vital for promoting mental health during the COVID-19 pandemic. During the short history of global mental health, there has already been an investment in building capacity in LMICs for research in the field.128, 129, 130 Additionally, there has been a substantial increase in research led by LMICs, and this is now influencing the way in which mental health care is envisaged in HICs.127 However, research priorities and programmes in global mental health are still too often led by funders and academics from HICs.131, 132 Research from LMICs is valued less in terms of strength of evidence and potential global impact, even when objectively rated as having equivalent quality.133 Addressing this bias requires HIC researchers, funders, and journal editors to embrace a position of humility, alongside challenging enduring colonial attitudes built into the education of LMIC professionals.134 In the face of the COVID-19 pandemic, the new norm must be mutual learning between all countries because even HICs are a long way from reaching universal and equitable coverage of mental health care.
Stakeholders: the who of global mental health
For both infectious disease and mental health, public health strategies fail when communities are not engaged with or are treated as passive recipients.135 Communities, including families of people with mental health conditions, local leadership, community health workers, and traditional and religious healers, must be empowered as active partners in delivering public health initiatives that are grounded in local realities and that recognise the interdependence of mental health, physical health, and social and economic context. Protecting mental health in the face of COVID-19 will be contingent on strategic coalitions and the development of collective pressure groups.
There have been some positive steps towards increased collaboration in global mental health, including evidence of effective collaboration between primary care workers and traditional and faith healers.136 However, global mental health advocates should become much firmer in demanding participatory action to implement community-led responses to the mental health impact of COVID-19, by taking advantage of a global climate where power structures are challenged, linking in with collective movements such as MeToo, Black Lives Matter, and student-led movements against environmental degradation.137 Young people's voices must be central to this endeavour, particularly given the potential long-term impact of the pandemic on their life chances. Similarly, the role of people with lived experience of mental ill health, their families and caregivers, and other groups at risk in shaping the systems that exist to serve their needs must go beyond nominal participation, recognising their unique perspective as experts by experience.138 Setting policy without meaningful engagement of individuals with lived experience as key stakeholders risks, at best, wasting resources on ineffective strategies and, at worst, causing harm.139, 140 People with lived experience have a key role in leading social contact anti-stigma interventions,141, 142 which is of particular relevance to efforts addressing intersecting the stigma related to COVID-19 and mental health. As the COVID-19 pandemic strains trust in authorities, localism becomes more important than ever as an effective approach to scaling up interventions.
The potential of peer support and further collaboration with people with lived experience of mental illness needs to be recognised within mental health-care systems, building on emerging initiatives (panel 1 ). Key lessons are to invest in capacity building for service users and to support peer workers to bring relational values to work (ie, offering equal, reciprocal relationships and taking a whole-of-life approach rather than one focused on illness). Currently, both LMICs and HICs have a long way to go in ensuring involvement of service users in research, policy, and programme implementation and evaluation.145, 146 For system change, there needs to be a conscious effort, backed by investment and policy, to equip and enable service users to be actively involved in all aspects of the system of care.147
Panel 1. Examples of service user partnership in the COVID-19 pandemic response.
- •
The Global Mental Health Peer Network, an international organisation for mental health service users, partnered with Human Rights in Mental Health–Federation Global Initiative on Psychiatry, an international organisation that promotes user-oriented mental health services, has advocated for greater equality and equity in the pandemic response through a joint position statement.143
- •
In a study that examined the psychosocial consequences of the pandemic, the Global Mental Health Peer Network collaborated with the World Dignity Project to carry out a global survey to ensure that the voices of people with lived experience of mental health, their families, and professionals who work with them are heard.144
- •
As a result of amplified needs for mental health support due to the pandemic, several mental health service user organisations have been involved in providing support. For example, the Psychiatric Disability Organization Kenya is providing psychosocial support for prison staff in Nakuru working in isolation, the Zimbabwe Obsessive Compulsive Disorder Trust is providing peer support addressing anxiety due to COVID-19, and the Global Mental Health Peer Network is running online COVID-19 and mental health virtual support groups twice monthly.
Sectors: the what of global mental health
To achieve good mental health as part of COVID-19 response efforts, we must ensure that people's basic needs are met and that human rights are protected. When social inequalities remain unaddressed, mental health interventions are less effective.148, 149 The pandemic response, including the mental health response, requires recognition of the syndemic co-occurrence and interaction of mental health, physical health, and social context (panel 2 ). Many of the social determinants of poor mental health, such as living in cramped conditions, scarce access to clean water and green spaces, poor nutrition, informal employment, and precarious working conditions, increase the risk of contracting SARS-CoV-2 and suffering complications after infection.156 Therefore, economic recovery packages should strategically address the social determinants that increase susceptibility to both COVID-19 and mental ill health. Across diverse settings, growing evidence indicates that national-level policies to improve the living conditions of low-paid workers and families can improve mental health at the population level.157, 158, 159 Social welfare, active labour market programmes that help people to retain or regain jobs, family support programmes, and debt support are all likely to help reduce the mental health impact of the crisis.160 In Latin America and Africa, governmental cash transfer programmes have documented positive mental health benefits, which could be more impactful than ever during the economic contraction caused by COVID-19.161 For example, greater coverage of the conditional cash transfer programme, Bolsa Família, in municipalities across Brazil was associated with reduced suicide rates.162 In Malawi's Social Cash Transfer Programme, depressive symptoms in young people were reduced by 15 percentage points, with the greatest benefits for those with the worst mental health.163, 164 Examples of other initiatives that have incorporated social and economic interventions into health programmes with important lessons for the crisis include the Atmiyata programme165 and the Society for Nutrition, Education, and Health Action's violence prevention interventions166 in India, Dream-a-World cultural therapy in Jamaica,167 the integrated intervention model for dialogue and screening in Kenya,168 and innovative nutrition programmes that simultaneously address violence, poverty, and mental distress in Ecuador.169
Panel 2. Applying syndemic theory to global mental health in the context of COVID-19.
Syndemic theory postulates that specific localised sociocultural, economic, and political conditions contribute to patterns of multimorbidity, and that settings without the same contextual features will not share these multimorbidity patterns.150, 151, 152 Syndemic theory goes beyond comorbidity to recognise the clustering of health burdens in a specific population that biologically interact to worsen health, and the shared sociostructural forces that exacerbate the biological disease interaction.150, 153 Therefore, diseases become concentrated in specific geographical or temporal contexts where people are exposed to harmful social conditions, interacting at individual and population levels to worsen health.
The ways in which, in some settings, COVID-19 is comorbid with high prevalence of non-communicable diseases, including cardiovascular, pulmonary, metabolic, and mental health conditions, and that these other conditions fall along gradients of economic and other disparities, suggests that there are different types of syndemics around the world, including in low-income and middle-income countries. There is not one universal COVID-19 syndemic, but rather context-specific interactions substantially aggravated in specific social groups and geographies.152 We cannot refer to a global COVID-19 syndemic, as the stark differences in disease pattern and response between countries like New Zealand and the USA clearly show. A nuanced and localised approach is crucial.
Approaching different local syndemics that involve COVID-19 highlights the need for integrated, intersectoral, and interdisciplinary responses. The interactions between substance misuse, violence, and HIV or AIDS154 led to the development of various multilevel interventions, including integrated behavioural interventions focusing on intimate partner violence and HIV prevention; integrated trauma-focused care to reduce substance misuse and post-traumatic stress disorder; synchronous community mobilisation interventions to reduce gender-based violence, HIV, and sexually transmitted illnesses (among men and women); and economic empowerment interventions to reduce gender-based violence and HIV risk.155 For COVID-19, taking a syndemic approach should similarly influence mental health responses and research, by recognising how biological and sociostructural factors interact to create mental health inequalities and by promoting a multilevel, intersectoral response that addresses the sociopolitical dynamics that lead to the clustering and interaction of poverty, infection, and mental ill health.150
Furthermore, inequality is an important determinant of mental health,170 and this is worsening as a result of the pandemic. Therefore, we must follow the Sustainable Development Goal principle of leaving no one behind and target interventions for the most marginalised groups. Such groups include people with severe mental illness or disabilities, communities living in extreme poverty, immigrants and displaced populations, and individuals who face discrimination for any reason.171, 172 The challenges of the COVID-19 pandemic further justify use of the principle of proportionate universalism,160 which focuses on protecting the rights and basic needs of young people (eg, enabling schools to open safely); reducing gender-based violence, which has escalated during the pandemic; and implementing environmental protection strategies, given the impact of environmental degradation on virus transmission and mental health.173
Building back better
The COVID-19 pandemic has affected mental health in all contexts and has highlighted the weaknesses of mental health systems globally. COVID-19 has shown the mental health impacts of pandemics not only on individuals with existing mental health needs but also across populations due to the polices aimed to stem its spread, which disproportionately affect vulnerable and already disadvantaged groups. It is vital that we recognise these effects as a historic opportunity to reimagine mental health systems, building on the vast body of clinical, implementation, and public health science119, 174 with the active engagement of all relevant stakeholders, particularly people with lived experience.
Building back better was a concept introduced in a report issued at the second anniversary of the 2004 Indian Ocean tsunami by the UN Secretary-General's Special Envoy for Tsunami Recovery, former US president, Bill Clinton.175 Since then, the concept has become the approach for nearly all post-disaster reconstruction programmes, including upending previously unchallenged and inadequate policies and practices. In 2013, the principles of building back better were used by WHO to provide a framework to support the development of sustainable post-disaster mental health systems, globally.176 Resource-limited countries, such as Afghanistan, Sri Lanka, Jordan, Nepal, and the occupied Palestinian territories, have shown how fragile mental health systems can be strengthened during and in the wake of public health emergencies.
The COVID-19 pandemic and the likelihood of future pandemics highlight the importance of resilient and responsive mental health systems.177 Although increased global and national investments in mental health were in great need even before the COVID-19 pandemic, there is a threat that the diversion of policy focus on the pandemic might further delay progress in mental health. We must work in concert with all stakeholders to ensure that resources are mobilised for strengthening mental health systems and that these investments are used in an effective and efficient manner, and cover the entire spectrum of needs, from promotion, protection, and prevention to treatment, care, and recovery. Reports from The Lancet Commission on global mental health and sustainable development119 and World Bank's Disease Control Priorities174 have outlined priorities for the strengthening of mental health systems. Within the context of COVID-19, we recommend a set of practical actions to address these priorities (panel 3 ).
Panel 3. Recommendations to build back better.
Integrating mental health services into UHC
Collaborative care strategies for building community capacity, based in primary care setup for community care and linkages with specialist services, is and must be the singular focus for investment.178 Collaborative care designs are essential in UHC and must be contextually appropriate and, through intersectoral partnerships, simultaneously address social and human rights concerns. It is essential to avoid impoverishment and catastrophic health-care costs in accessing mental health care.
Improving access and coverage of psychosocial interventions
A crucial aspect of UHC for mental health care is the community delivery of psychosocial interventions by front-line providers, such as community health workers and peers (ie, task-sharing interventions). These providers are needed for addressing mental health issues related to COVID-19 and for deploying a host of innovations, such as digital training and competency assessment, peer supervision, and quantifiable quality metrics, to help build a workforce to address prevention and treatment gaps.179, 180, 181, 182
Eliminating coercion in mental health care
The Convention on the Rights of Persons with Disabilities has laid down the foundational values of a world in which coercion must be abolished in all aspects of health care and for all people, and has developed various strategies to support decision making, rather than substitute it.183 A crucial element is engagement of people with lived experience. Peer support activities are associated with improved treatment outcomes and promotion of human rights.184, 185 These strategies are essential during the COVID-19 pandemic for the inclusion of individuals with mental health conditions in the design and implementation of services.186, 187
Integrating mental health interventions into other sectors
COVID-19 has amply shown the interdependence of health and other sectors.188 The relationships between mental health and gender, education, employment, and social networks is attracting fresh policy attention in the face of unprecedented worsening of poverty and inequality in the near future. Intersectoral strategies are essential for sustainable recovery from mental disorders, and for addressing stigma and other negative consequences associated with health seeking119 for overall reduction in the incidence of new cases.
Addressing the mental health of children and young people
One blind spot of global mental health has been its relative neglect of children and young people (aged <24 years). More than 80% of the world's young people live in low-income and middle-income countries. Given how the complete closure of schools and colleges is directly affecting the lives of young people, building back better with intersectional approaches must explicitly address this crucially important demographic group to promote nurturing environments at home, in schools, and across neighbourhoods.189
Incorporating technological innovations in mental health services
The COVID-19 pandemic has fuelled a striking transformation in the use of digital platforms for various mental health-care tasks. The opportunities presented by use of digital technology could address stigma and discrimination, isolation and marginalisation; identify individuals at risk (through social media footprints); and assist with the training and supervision of front-line workers. However, caution is needed so that its use does not increase the existing disparities in access. Use of personal digital information also needs to be done in accordance with local regulations and in a way that maximises protection of privacy and confidentiality.190
UHC=universal health coverage.
Conclusions
The COVID-19 pandemic has disrupted every aspect of life in all countries almost simultaneously and, in this respect, represents a global phenomenon unlike any other in human history. Emerging evidence indicates that the mental health impacts will be large, long-lasting, and greatest in under-resourced contexts and disadvantaged populations. Unless addressed robustly and urgently, these impacts will contribute to enormous human suffering, premature mortality, and social breakdown, and will slow down economic recovery. Although there was already an enormous crisis relating to mental health before the pandemic, COVID-19 presents an historic opportunity for all countries and global agencies to reassess how human society organises itself to recover from these impacts. We know what this should look like; not only should we invest in building mental health systems now but we should also ensure that these investments embrace the diversity of experiences and actions that characterise mental ill health, well beyond the narrow biomedical focus on doctors, diagnoses, and drugs that has dominated mental health policies globally. Thus, we call for a balanced approach that addresses the social determinants of mental health and the individual clinical needs for people with mental health disorders. Mental health interventions that fail to take account of social determinants of mental ill health, especially those exacerbated by COVID-19, will fail to achieve their intended impacts. With a balanced approach, we can not only reimagine mental health care in LMICs, but also reframe mental health as a common and prioritised aspiration in all countries worldwide.
Search strategy and selection criteria
Section leads searched the peer-reviewed literature on PubMed for articles published between Jan 1 and July 31, 2020, describing the impact of the COVID-19 pandemic on mental health using the search terms “mental health”, “depression”, “anxiety”, “psychosis”, “schizophrenia”, “posttraumatic stress disorder”, “suicide”, “substance use disorders”, “alcohol use disorders”, or “child and adolescent mental health” and “COVID-19”. The search was restricted to articles published in English. We used the current fiscal-year classifications of World Bank Country and Lending Groups and included low-income, lower-middle-income, and upper-middle-income countries on the basis of 2019 economic data. Given that research on this topic continues to evolve rapidly and, to date, there have been relatively few studies published from low-income and middle-income countries, we broadened our search to Google searches and contacted key informants (including the large and globally representative group of authors of this Review). We reviewed reports and guidance from WHO, the Inter-Agency Standing Committee, MHPSS.net and mhinnovation.net, and reached out to non-governmental organisations in low-income and middle-income countries. The resulting literature was summarised and interrogated by our authorship group, which included senior global mental health experts, and relevant content was synthesised through multiple rounds of feedback and review.
This online publication has been corrected. The corrected version first appeared at thelancet.com/psychiatry on March 8, 2021.
Acknowledgments
Acknowledgments
The authors thank Amir Afkhami, Kenneth Carswell, Carmen Contreras, Benedict Dossen, Wilfred Gwaikolo, Christian Kieling, Crick Lund, Byamah Mutamba, Alison Schafer, and Katherine Sorsdahl for sharing valuable information about COVID-19 mental health response plans, programmes, and resources. No funding was provided to support this Review.
Contributors
LK and VP conceptualised and drafted the full manuscript. BAK, CH, JAN, and SS led the drafting of each of the four major sections of the paper. BAK developed the figures. All authors reviewed and approved the final version of the paper.
Declaration of interests
VP and SSa are co-founders of Librum, a mental health consulting company. TTS reports grant funding from the UK Medical Research Council, Bill & Melinda Gates Foundation, and UK Research and Innovation. TTS also reports consultancy income for mental health research from Save the Children Denmark and The MHPSS Collaborative, and travel to a mental health conference paid by the Tunisian Government. CB reports grants from the US National Institutes of Health. LK is supported by the US National Institute of Mental Health (NIMH; K43TW011046). BAK is supported by the US NIMH (R01MH120649). CH and GT are funded by the National Institute of Health Research (NIHR) Global Health Research Unit on Health System Strengthening in Sub-Saharan Africa, King's College London (GHRU 16/136/54) using UK aid from the UK Government. CH receives support from AMARI as part of the DELTAS Africa Initiative [DEL-15-01]. GT is supported by the NIHR Applied Research Collaboration South London at King's College London NHS Foundation Trust. GT also receives support from the NIMH of the National Institutes of Health under award number R01MH100470 (Cobalt study). GT is supported by the UK Medical Research Council in relation to the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards. JE is supported by the UK Foreign, Commonwealth and Development Office through the SUCCEED Research Programme Consortium at London School of Hygiene and Tropical Medicine. MB is supported by the Wellcome Trust/DBT India Alliance. TTS is supported by a UK Research and Innovation Future Leaders Fellow award. TR is supported by a UK Economic and Social Research Council fellowship (ES/T007125/1). JAN and VP are supported by the US NIMH (5U19MH113211). The views expressed are those of the authors and not necessarily those of the NIMH, NHS, the NIHR, UK Department of Health and Social Care, or any other funder. All other authors declare no competing interests.
References
- 1.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liese BH, Gribble RSF, Wickremsinhe MN. International funding for mental health: a review of the last decade. Int Health. 2019;11:361–369. doi: 10.1093/inthealth/ihz040. [DOI] [PubMed] [Google Scholar]
- 4.Jordan RE, Adab P, Cheng KK. COVID-19: risk factors for severe disease and death. BMJ. 2020;368 doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 5.Rosengren A, Smyth A, Rangarajan S, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7:e748–e760. doi: 10.1016/S2214-109X(19)30045-2. [DOI] [PubMed] [Google Scholar]
- 6.Sarki AM, Nduka CU, Stranges S, Kandala N-B, Uthman OA. Prevalence of hypertension in low- and middle-income countries: a systematic review and meta-analysis. Medicine (Baltimore) 2015;94 doi: 10.1097/MD.0000000000001959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geldsetzer P, Manne-Goehler J, Marcus ME, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1·1 million adults. Lancet. 2019;394:652–662. doi: 10.1016/S0140-6736(19)30955-9. [DOI] [PubMed] [Google Scholar]
- 8.Mahler D, Lakner C, Aguilar C, Wu H. Updated estimates of the impact of COVID-19 on global poverty. June 8, 2020. https://blogs.worldbank.org/opendata/updated-estimates-impact-covid-19-global-poverty
- 9.Altiraifi A, Rapfogel N. Mental health care was severely inequitable, then came the coronavirus crisis. Sept 10, 2020. https://www.americanprogress.org/issues/disability/reports/2020/09/10/490221/mental-health-care-severely-inequitable-came-coronavirus-crisis/
- 10.Kola L. Global mental health and COVID-19. Lancet Psychiatry. 2020;7:655–657. doi: 10.1016/S2215-0366(20)30235-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Sousa A, Mohandas E, Javed A. Psychological interventions during COVID-19: challenges for low and middle income countries. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vigo D, Thornicroft G, Gureje O. The differential outcomes of coronavirus disease 2019 in low- and middle-income countries vs high-income countries. JAMA Psychiatry. 2020;77:1207–1208. doi: 10.1001/jamapsychiatry.2020.2174. [DOI] [PubMed] [Google Scholar]
- 13.The World Bank Word Bank country and lending groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups#:~:text=For%20the%20current%202021%20fiscal,those%20with%20a%20GNI%20per
- 14.Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113:531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. 2020;20:782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mamun MA, Sakib N, Gozal D, et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J Affect Disord. 2020;279:462–472. doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vigo D, Patten S, Pajer K, et al. Mental health of communities during the COVID-19 pandemic. Can J Psychiatry. 2020 doi: 10.1177/0706743720926676. published online May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gureje O. Coronavirus disease 2019 pandemic in low and middle income countries: the pivotal place of social psychiatry. World Social Psychiatry. 2020;2:94–96. [Google Scholar]
- 20.Mukhopadhyay A. Police under fire for using violence to enforce coronavirus lockdown. March 28, 2020. https://www.dw.com/en/india-police-under-fire-for-using-violence-to-enforce-coronavirus-lockdown/a-52946717
- 21.Farge E. U.N. raises alarm about police brutality in lockdowns. April 27, 2020. https://www.reuters.com/article/us-health-coronavirus-un-rights/u-n-raises-alarm-about-police-brutality-in-lockdowns-idUSKCN2291X9
- 22.Mkhwanazi S. 49 cases of police brutality reported since start of lockdown, says Bheki Cele. June 30, 2020. https://www.iol.co.za/news/politics/49-cases-of-police-brutality-reported-since-start-of-lockdown-says-bheki-cele-50160784
- 23.Onubogu O. COVID-19 and conflict: Nigeria. May 28, 2020. https://www.usip.org/blog/2020/05/covid-19-and-conflict-nigeria
- 24.Bearak M. Amid a corruption scandal over coronavirus supplies, Zimbabwe cracks down on critics. July 21, 2020. https://www.washingtonpost.com/world/africa/zimbabwe-detains-prominent-journalist-activist-who-called-for-mass-protests/2020/07/21/42c8e958-cb23-11ea-99b0-8426e26d203b_story.html
- 25.Marima T. Anxiety over rights violations as Zimbabwe enforces lockdown. April 6, 2020. https://www.aljazeera.com/news/2020/4/6/anxiety-over-rights-violations-as-zimbabwe-enforces-lockdown
- 26.Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during COVID-19 pandemic restrictions. BMJ. 2020;369 doi: 10.1136/bmj.m1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lund C, Brooke-Sumner C, Baingana F, et al. Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Lancet Psychiatry. 2018;5:357–369. doi: 10.1016/S2215-0366(18)30060-9. [DOI] [PubMed] [Google Scholar]
- 28.Javed B, Sarwer A, Soto EB, Mashwani ZU. Impact of SARS-CoV-2 (Coronavirus) pandemic on public mental health. Front Public Health. 2020;8:292. doi: 10.3389/fpubh.2020.00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maroko A, Nash D, Pavilonis B. COVID-19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J Urban Health. 2020;97:461–470. doi: 10.1007/s11524-020-00468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Afifi RA, Novak N, Gilbert PA, et al. ‘Most at risk’ for COVID19? The imperative to expand the definition from biological to social factors for equity. Prev Med. 2020;139 doi: 10.1016/j.ypmed.2020.106229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Castro-de-Araujo LFS, Machado DB. Impact of COVID-19 on mental health in a low and middle-income country. Cien Saude Colet. 2020;25(suppl 1):2457–2460. doi: 10.1590/1413-81232020256.1.10932020. [DOI] [PubMed] [Google Scholar]
- 33.Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019—a perfect storm? JAMA Psychiatry. 2020;77 doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- 34.Castro-de-Araujo LFS, Machado DB. Impacto do COVID-19 na saúde mental em um país de baixa e média renda. Cien Saude Colet. 2020;25:2457–2460. doi: 10.1590/1413-81232020256.1.10932020. [DOI] [PubMed] [Google Scholar]
- 35.Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang L, Yin J, Wang D, Rahman A, Li X. Urgent need to develop evidence-based self-help interventions for mental health of healthcare workers in COVID-19 pandemic. Psychol Med. 2020 doi: 10.1017/S0033291720001385. published online April 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ballard M, Bancroft E, Nesbit J, et al. Prioritising the role of community health workers in the COVID-19 response. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nagesh S, Chakraborty S. Saving the frontline health workforce amidst the COVID-19 crisis: challenges and recommendations. J Glob Health. 2020;10 doi: 10.7189/jogh-10-010345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang C, Yang L, Liu S, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Whiteford H, Ferrari A, Degenhardt L. Global Burden Of Disease studies: implications for mental and substance use disorders. Health Aff (Millwood) 2016;35:1114–1120. doi: 10.1377/hlthaff.2016.0082. [DOI] [PubMed] [Google Scholar]
- 43.Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7:389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McIntyre RS, Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020;19:250–251. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ. 2019;364:l94. doi: 10.1136/bmj.l94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Balaji M, Patel V. Hunger, fear and isolation: an analysis of media reports of COVID-19 related suicides in India. Research Square. 2020 doi: 10.21203/rs.3.rs-99851/v1. published online Oct 30. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jordans M, Rathod S, Fekadu A, et al. Suicidal ideation and behaviour among community and health care seeking populations in five low- and middle-income countries: a cross-sectional study. Epidemiol Psychiatr Sci. 2018;27:393–402. doi: 10.1017/S2045796017000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hagaman AK, Maharjan U, Kohrt BA. Suicide surveillance and health systems in Nepal: a qualitative and social network analysis. Int J Ment Health Syst. 2016;10:46. doi: 10.1186/s13033-016-0073-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112:15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Joseph SJ, Bhandari SS, Ranjitkar S, Dutta S. School closures and mental health concerns for children and adolescents during the covid-19 pandemic. Psychiatr Danub. 2020;32:309–310. [PMC free article] [PubMed] [Google Scholar]
- 51.Wang D, Fawzi WW. Impacts of school feeding on educational and health outcomes of school-age children and adolescents in low- and middle-income countries: protocol for a systematic review and meta-analysis. Syst Rev. 2020;9:55. doi: 10.1186/s13643-020-01317-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Adelman S, Gilligan D, Lehrer K. International Food Policy Research Institute; Washington, DC: 2008. How effective are food for education programs? A critical assessment of the evidence from developing countries. [Google Scholar]
- 53.Aliyar R, Gelli A, Hamdani SH. A review of nutritional guidelines and menu compositions for school feeding programs in 12 countries. Front Public Health. 2015;3:148. doi: 10.3389/fpubh.2015.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Van Lancker W, Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. Lancet Public Health. 2020;5:e243–e244. doi: 10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Inter-Agency Standing Committee Interim briefing note addressing mental health and psychosocial aspects of COVID-19 outbreak (developed by the IASC's Reference Group on Mental Health and Psychosocial Support) https://interagencystandingcommittee.org/iasc-reference-group-mental-health-and-psychosocial-support-emergency-settings/interim-briefing
- 56.International Federation of Red Cross and Red Crescent Societies. UNICEF. WHO A guide to preventing and addressing social stigma associated with COVID-19. Feb 24, 2020. https://www.who.int/publications/m/item/a-guide-to-preventing-and-addressing-social-stigma-associated-with-covid-19
- 57.Li W, Yang Y, Liu Z-H, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16:1732–1738. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.International Federation of Red Cross and Red Crescent Societies Remote psychological first aid during a COVID-19 outbreak. March 2020. https://pscentre.org/wp-content/uploads/2020/03/IFRC-PS-Centre.-Remote-PFA-during-a-COVID-19-outbreak.-Final.-ENG.pdf
- 59.International Organization for Migration . International Organization for Migration; Geneva: 2020. Mental health and psychosocial support (MHPSS) in the COVID-19 response: guidance and toolkit for the use of IOM MHPSS Teams: version II. [Google Scholar]
- 60.Inter-Agency Standing Committee My hero is you, storybook for children on COVID-19. https://www.unicef.org/coronavirus/my-hero-you
- 61.Republic of Lebanon Ministry of Public Health National action plan for the MHPSS response to COVID-19. https://www.moph.gov.lb/en/Pages/6/29466/action-plan-mentalhealth-covid19
- 62.Republic of South Africa Guidelines on mental health interventions during the COVID-19 disaster. March 31, 2020. https://www.westerncape.gov.za/assets/departments/health/COVID-19/guidelines_on_mental_health_interventions_during_the_covid-19_disaster.pdf
- 63.Ministry of Health A comprehensive guide on mental health and psychosocial support during the COVID-19 pandemic. https://www.health.go.ke/wp-content/uploads/2020/04/Final-Comprehensive-Guide-on-Mental-Health-and-Psychosocial-Support-For-COVID-19-Pandemic-4.pdf
- 64.Ministry of Health . Government of Uganda; Kampala: 2020. COVID-19 response plan. [Google Scholar]
- 65.Malsa M. COVID-19: Maldives establishes mental and psychological cluster. April 28, 2020. https://edition.mv/news/16420
- 66.Department of Psychiatry National Institute of Mental Health & Neurosciences . Department of Psychiatry National Institute of Mental Health & Neurosciences; Bengaluru: 2020. Mental health in the times of COVID-19 pandemic guidance for general medical and specialised mental health care settings. [Google Scholar]
- 67.WHO . World Health Organization; Geneva: 2020. Doing what matters in times of stress: an illustrated guide. [Google Scholar]
- 68.Kohrt BA, Schafer A, Willhoite A, et al. Ensuring Quality in Psychological Support (WHO EQUIP): developing a competent global workforce. World Psychiatry. 2020;19:115–116. doi: 10.1002/wps.20704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mental Health Information Network. WHO Stories from the field: providing mental health and psychosocial support during the COVID-19 pandemic. https://www.mhinnovation.net/stories-field-providing-mental-health-and-psychosocial-support-during-covid-19-pandemic
- 70.UN Policy brief: COVID-19 and the need for action on mental health. May 13, 2020. https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf
- 71.Africa Centres for Disease Control and Prevention Guidance for mental health and psychosocial support for COVID-19. https://africacdc.org/download/guidance-for-mental-health-and-psychosocial-support-for-covid-19/
- 72.WHO . World Health Organization; Geneva: 2020. Clinical management of COVID-19: interim guidance. [Google Scholar]
- 73.WHO . World Health Organization; Geneva: 2020. Maintaining essential health services: operational guidance for the COVID-19 context. [Google Scholar]
- 74.Inter-Agency Standing Committee Basic psychosocial skills: a guide for COVID-19 responders. May 26, 2020. https://interagencystandingcommittee.org/iasc-reference-group-mental-health-and-psychosocial-support-emergency-settings/iasc-guidance-basic-psychosocial-skills-guide-covid-19-responders
- 75.International Federation of Red Cross and Red Crescent Societies COVID-19 response update #3. https://go.ifrc.org/reports/12926 [DOI] [PubMed]
- 76.Eaton J, Rahman A, Gater R, Saxena S, Hammerich A, Saeed K. From adversity to resilience in the COVID-19 era: strengthening mental health systems in the Eastern Mediterranean Region. East Mediterr Health J. 2020;26:1148–1150. doi: 10.26719/2020.26.10.1148. [DOI] [PubMed] [Google Scholar]
- 77.Papola D, Purgato M, Gastaldon C, et al. Psychological and social interventions for the prevention of mental disorders in people living in low- and middle-income countries affected by humanitarian crises. Cochrane Database Syst Rev. 2020;9 doi: 10.1002/14651858.CD012417.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Upadhaya N, Luitel NP, Koirala S, et al. The role of mental health and psychosocial support nongovernmental organizations: reflections from post-conflict Nepal. Intervention. 2014;12(suppl 1):113–128. [Google Scholar]
- 79.Inter-Agency Standing Committee . Inter-Agency Standing Committee; Geneva: 2007. Guidelines on mental health and psychosocial support in emergency settings. [DOI] [PubMed] [Google Scholar]
- 80.Inter-Agency Standing Committee Reference Group for Mental Health and Psychosocial Support in Emergency Settings . Inter-Agency Standing Committee; Geneva: 2012. Who is where, when, doing what (4ws) in mental health and psychosocial support: manual with activity codes. [Google Scholar]
- 81.WHO . World Health Organization; Geneva: 2012. Assessing mental health and psychosocial needs and resources: toolkit for humanitarian settings. [Google Scholar]
- 82.Hobfoll SE, Watson P, Bell CC, et al. Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry. 2007;70:283–315. doi: 10.1521/psyc.2007.70.4.283. [DOI] [PubMed] [Google Scholar]
- 83.John CE, Gunasekaran I, Maria NR. COVID-19: taking heed from Kerala's mental health interventions. March 27, 2020. https://science.thewire.in/health/covid-19-kerala-mental-health/
- 84.Borah PM. COVID-19: a little act of kindness can #sparkthejoy. April 25, 2020. https://www.thehindu.com/society/little-act-of-kindness-can-sparkthejoy/article31430300.ece
- 85.Express News Service Kindness bingo, anyone? This campaign was to engage the user and derive better mental health and positivity for users. May 28, 2020. https://www.newindianexpress.com/cities/hyderabad/2020/may/28/kindness-bingo-anyone-2148844.html
- 86.Ralston AL, Andrews AR, 3rd, Hope DA. Fulfilling the promise of mental health technology to reduce public health disparities: review and research agenda. Clin Psychol Sci Pract. 2019;26 [Google Scholar]
- 87.Narayanan D. Is Kerala's well-managed COVID-19 fight threatening to unravel? July 5, 2020. https://economictimes.indiatimes.com/news/politics-and-nation/is-keralas-well-managed-covid-19-fight-threatening-to-unravel/articleshow/76788706.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst
- 88.Yasmeen F. BasicNeeds Pakistan: supporting mental health in under-resourced communities during the COVID-19 pandemic. May 12, 2020. https://www.mhinnovation.net/blog/2020/may/12/basicneeds-pakistan-supporting-mental-health-under-resourced-communities-during
- 89.Partners in Health As COVID-19 cases mount in Peru, medical and social support are key. July 8, 2020. https://www.pih.org/article/covid-19-cases-mount-peru-medical-and-social-support-are-key
- 90.Sabatello M, Burke TB, McDonald KE, Appelbaum PS. Disability, ethics, and health care in the COVID-19 pandemic. Am J Public Health. 2020;110:1523–1527. doi: 10.2105/AJPH.2020.305837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tuna O, Enez Darcin A, Tarakcioglu MC, Aksoy UM. COVID-19 Positive Psychiatry Inpatient Unit: a unique experience. Asia Pac Psychiatry. 2020 doi: 10.1111/appy.12410. published online Aug 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Puglisi F. South Africa's mental health care falls by wayside during pandemic. May 27, 2020. https://www.voanews.com/africa/south-africas-mental-health-care-falls-wayside-during-pandemic
- 93.Badrfam R, Zandifar A. COVID-19 and mental health: an Iranian perspective. Asian J Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Frontières MS. MSF “deeply surprised” that Iranian authorities put a stop to our COVID-19 response. March 25, 2020. https://www.msf.org/msf-surprised-iran-put-stop-our-covid-19-response
- 95.Nadkarni A, Kapoor A, Pathare S. COVID-19 and forced alcohol abstinence in India: the dilemmas around ethics and rights. Int J Law Psychiatry. 2020;71 doi: 10.1016/j.ijlp.2020.101579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Anand A. Goa starts counselling for migrant labourers. April 6, 2020. https://www.thehindu.com/news/states/goa-starts-counselling-for-migrant-labourers/article31265387.ece
- 97.Directorate of Information Public Relations OOAT clinics and all de-addiction centres to provide take-home dose for 2 weeks to registered patients: Balbir Singh Sidhu. March 29, 2020. http://diprpunjab.gov.in/?q=content/ooat-clinics-all-de-addiction-centres-provide-take-home-dose-2-weeks-registered-patients
- 98.Salum GA, Rehmenklau JF, Csordas MC, et al. Supporting people with severe mental health conditions during the COVID-19 pandemic: considerations for low- and middle-income countries using telehealth case management. Braz J Psychiatry. 2020;42:451–452. doi: 10.1590/1516-4446-2020-1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cappo MD, Mutamba BB. “We do not know how to face it when it comes!” A rapid COVID-19 related phone survey of individuals and families who have been supported by the YouBelong Uganda community based mental health programme in Kampala and Wakiso Districts, Uganda. https://youbelongcommunity.org/wp-content/uploads/2020/05/COVID-19-Phone-Survey-YouBelong-Uganda.pdf
- 100.Kaligis F, Indraswari MT, Ismail RI. Stress during COVID-19 pandemic: mental health condition in Indonesia. Med J Indones. 2020;29:436–441. [Google Scholar]
- 101.Ghosh S. Mental health matters: why young India is depressed and anxious about life in a post-COVID world. June 25, 2020. https://www.edexlive.com/opinion/2020/jun/25/mental-health-matters-why-young-india-is-depressed-and-anxious-about-life-in-a-post-covid-world-12875.html
- 102.Joshi S. Online health platforms see spike in mental health queries amidst COVID-19 pandemic. June 25, 2020. https://timesofindia.indiatimes.com/home/sunday-times/online-health-platforms-see-spike-in-mental-health-queries-amidst-covid-19-pandemic/articleshow/76630185.cms
- 103.Gbenga AM. COVID-19 and mental health: Jolade Phillips of Mani speaks on the pandemic and how to stay mentally healthy. May 8, 2020. http://venturesafrica.com/covid-19-and-mental-health-live-session-with-jolade-phillips-communications-lead-at-mentally-aware-nigeria-initiative/
- 104.Tomacruz S. NCMH records spike in mental health consults during coronavirus lockdown. June 8, 2020. https://rappler.com/nation/national-center-mental-health-records-spike-hotline-calls-during-coronavirus-lockdown
- 105.Sinkins E. Providing mental health support for frontline workers. June 8, 2020. https://www.news24.com/news24/southafrica/news/providing-mental-health-support-for-frontline-workers-20200608-2
- 106.Dawson KS, Bryant RA, Harper M, et al. Problem Management Plus (PM+): a WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry. 2015;14:354–357. doi: 10.1002/wps.20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.McBride K. International Federation of Red Cross and Red Crescent Societies: Psychosocial Centre; Copenhagen: 2020. Remote PM+ training of helpers: training & lessons learned report. [Google Scholar]
- 108.Friendship Bench Digital trial. 2020. https://www.friendshipbenchzimbabwe.org/digital-trial
- 109.Armitage R, Nellums LB. The COVID-19 response must be disability inclusive. Lancet Public Health. 2020;5:e257. doi: 10.1016/S2468-2667(20)30076-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Aga Khan University Pakistan COVID-19 mental health response for children and adolescents. 2020. https://www.aku.edu/covid-mental-health-response/Pages/home.aspx
- 111.Cooper JL. Mental health and psychosocial support in the face of Ebola in Liberia: the personal and professional intersect. A personal account. Intervention (Amstelveen) 2015;13:49–57. [Google Scholar]
- 112.Weissbecker I, Roshania R, Cavallera V, et al. Integrating psychosocial support at Ebola treatment units in Sierra Leone and Liberia. Intervention (Amstelveen) 2018;16:69–78. [Google Scholar]
- 113.Cheung E. An outbreak of fear, rumours and stigma: psychosocial support for the Ebola Virus Disease outbreak in West Africa. Intervention (Amstelveen) 2015;13:70–76. [Google Scholar]
- 114.Alonge O, Sonkarlay S, Gwaikolo W, Fahim C, Cooper JL, Peters DH. Understanding the role of community resilience in addressing the Ebola virus disease epidemic in Liberia: a qualitative study (community resilience in Liberia) Glob Health Action. 2019;12 doi: 10.1080/16549716.2019.1662682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.WHO. CBM. World Vision. UNICEF . World Health Organization; Geneva: 2014. Facilitation manual: psychological first aid during Ebola virus disease outbreaks. [Google Scholar]
- 116.Dean L, Cooper J, Wurie H, et al. Psychological resilience, fragility and the health workforce: lessons on pandemic preparedness from Liberia and Sierra Leone. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kohrt BA, Blasingame E, Compton MT, et al. Adapting the Crisis Intervention Team (CIT) model of police-mental health collaboration in a low-income, post-conflict country: curriculum development in Liberia, West Africa. Am J Public Health. 2015;105:e73–e80. doi: 10.2105/AJPH.2014.302394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Pathare S, Brazinova A, Levav I. Care gap: a comprehensive measure to quantify unmet needs in mental health. Epidemiol Psychiatr Sci. 2018;27:463–467. doi: 10.1017/S2045796018000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Patel V, Saxena S, Lund C, et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392:1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- 120.Johns Hopkins Coronavirus Resource Center Mortality analyses. https://coronavirus.jhu.edu/data/mortality
- 121.Gureje O, Nortje G, Makanjuola V, Oladeji BD, Seedat S, Jenkins R. The role of global traditional and complementary systems of medicine in the treatment of mental health disorders. Lancet Psychiatry. 2015;2:168–177. doi: 10.1016/S2215-0366(15)00013-9. [DOI] [PubMed] [Google Scholar]
- 122.Kohrt BA, Asher L, Bhardwaj A, et al. The role of communities in mental health care in low- and middle-income countries: a meta-review of components and competencies. Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15061279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pham TV, Koirala R, Wainberg ML, Kohrt BA. Reassessing the mental health treatment gap: what happens if we include the impact of traditional healing on mental illness? Community Ment Health J. 2020 doi: 10.1007/s10597-020-00705-5. published online Sept 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kottai SR, Ranganathan S. Task-shifting in community mental health in Kerala: tensions and ruptures. Med Anthropol. 2020;39:538–552. doi: 10.1080/01459740.2020.1722122. [DOI] [PubMed] [Google Scholar]
- 126.Gautier L, Sieleunou I, Kalolo A. Deconstructing the notion of “global health research partnerships” across Northern and African contexts. BMC Med Ethics. 2018;19(suppl 1):49. doi: 10.1186/s12910-018-0280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Breuer E, Hanlon C, Bhana A, et al. Partnerships in a global mental health research programme—the example of PRIME. Glob Soc Welf. 2019;6:159–175. doi: 10.1007/s40609-018-0128-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Chibanda D, Abas M, Musesengwa R, et al. Mental health research capacity building in sub-Saharan Africa: the African Mental Health Research Initiative. Glob Ment Health (Camb) 2020;7:e8. doi: 10.1017/gmh.2019.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Schneider M, Sorsdahl K, Mayston R, et al. Developing mental health research in sub-Saharan Africa: capacity building in the AFFIRM project. Glob Ment Health (Camb) 2016;3:e33. doi: 10.1017/gmh.2016.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gureje O, Seedat S, Kola L, et al. Partnership for mental health development in Sub-Saharan Africa (PaM-D): a collaborative initiative for research and capacity building. Epidemiol Psychiatr Sci. 2019;28:389–396. doi: 10.1017/S2045796018000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hedt-Gauthier BL, Jeufack HM, Neufeld NH, et al. Stuck in the middle: a systematic review of authorship in collaborative health research in Africa, 2014-2016. BMJ Glob Health. 2019;4 doi: 10.1136/bmjgh-2019-001853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Abimbola S. The foreign gaze: authorship in academic global health. BMJ Global Health. 2019;4 doi: 10.1136/bmjgh-2019-002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Harris M, Marti J, Watt H, Bhatti Y, Macinko J, Darzi AW. Explicit bias toward high-income-country research: a randomized, blinded, crossover experiment of English clinicians. Health Aff (Millwood) 2017;36:1997–2004. doi: 10.1377/hlthaff.2017.0773. [DOI] [PubMed] [Google Scholar]
- 134.The Lancet Psychiatry The end, and the beginning, of global mental health. Lancet Psychiatry. 2020;7:538–546. doi: 10.1016/S2215-0366(20)30348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wilkinson A, Parker M, Martineau F, Leach M. Engaging ‘communities’: anthropological insights from the West African Ebola epidemic. Philos Trans R Soc Lond B Biol Sci. 2017;372 doi: 10.1098/rstb.2016.0305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gureje O, Appiah-Poku J, Bello T, et al. Effect of collaborative care between traditional and faith healers and primary health-care workers on psychosis outcomes in Nigeria and Ghana (COSIMPO): a cluster randomised controlled trial. Lancet. 2020;396:612–622. doi: 10.1016/S0140-6736(20)30634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Weine S, Kohrt BA, Collins PY, et al. Justice for George Floyd and a reckoning for global mental health. Glob Ment Health (Camb) 2020;7:e22. doi: 10.1017/gmh.2020.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Gillard S, Borschmann R, Turner K, Goodrich-Purnell N, Lovell K, Chambers M. ‘What difference does it make?’ Finding evidence of the impact of mental health service user researchers on research into the experiences of detained psychiatric patients. Health Expect. 2010;13:185–194. doi: 10.1111/j.1369-7625.2010.00596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Thornicroft G, Tansella M. Growing recognition of the importance of service user involvement in mental health service planning and evaluation. Epidemiol Psichiatr Soc. 2005;14:1–3. doi: 10.1017/s1121189x00001858. [DOI] [PubMed] [Google Scholar]
- 140.Hanlon C, Semrau M, Alem A, et al. Evaluating capacity-building for mental health system strengthening in low- and middle-income countries for service users and caregivers, service planners and researchers. Epidemiol Psychiatr Sci. 2018;27:3–10. doi: 10.1017/S2045796017000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Thornicroft G, Mehta N, Clement S, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387:1123–1132. doi: 10.1016/S0140-6736(15)00298-6. [DOI] [PubMed] [Google Scholar]
- 142.Kohrt BA, Turner EL, Rai S, et al. Reducing mental illness stigma in healthcare settings: proof of concept for a social contact intervention to address what matters most for primary care providers. Soc Sci Med. 2020;250 doi: 10.1016/j.socscimed.2020.112852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Global Mental Health Peer Network. Federation Global Initiative on Psychiatry Joint equality & equity in COVID19 response. https://www.gmhpn.org/uploads/1/2/0/2/120276896/gmhpn___fgip_joint_position_statement_-_covid19.pdf
- 144.Ivbijaro G, Brooks C, Kolkiewicz L, Sunkel C, Long A. Psychological impact and psychosocial consequences of the COVID 19 pandemic Resilience, mental well-being, and the coronavirus pandemic. Indian J Psychiatry. 2020;62(suppl 3):S395–S403. doi: 10.4103/psychiatry.IndianJPsychiatry_1031_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Semrau M, Lempp H, Keynejad R, et al. Service user and caregiver involvement in mental health system strengthening in low- and middle-income countries: systematic review. BMC Health Serv Res. 2016;16:79. doi: 10.1186/s12913-016-1323-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ryan GK, Semrau M, Nkurunungi E, Mpango RS. Service user involvement in global mental health: what have we learned from recent research in low and middle-income countries? Curr Opin Psychiatry. 2019;32:355–360. doi: 10.1097/YCO.0000000000000506. [DOI] [PubMed] [Google Scholar]
- 147.Lempp H, Abayneh S, Gurung D, et al. Service user and caregiver involvement in mental health system strengthening in low- and middle-income countries: a cross-country qualitative study. Epidemiol Psychiatr Sci. 2018;27:29–39. doi: 10.1017/S2045796017000634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Finegan M, Firth N, Wojnarowski C, Delgadillo J. Associations between socioeconomic status and psychological therapy outcomes: a systematic review and meta-analysis. Depress Anxiety. 2018;35:560–573. doi: 10.1002/da.22765. [DOI] [PubMed] [Google Scholar]
- 149.Elwadhi D, Cohen A. Social inequalities in antidepressant treatment outcomes: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2020;55:1241–1259. doi: 10.1007/s00127-020-01918-5. [DOI] [PubMed] [Google Scholar]
- 150.Mendenhall E, Kohrt BA, Norris SA, Ndetei D, Prabhakaran D. Non-communicable disease syndemics: poverty, depression, and diabetes among low-income populations. Lancet. 2017;389:951–963. doi: 10.1016/S0140-6736(17)30402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kohrt BA, Carruth L. Syndemic effects in complex humanitarian emergencies: a framework for understanding political violence and improving multi-morbidity health outcomes. Soc Sci Med. 2020 doi: 10.1016/j.socscimed.2020.113378. published online Sept 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Mendenhall E. The COVID-19 syndemic is not global: context matters. Lancet. 2020;396 doi: 10.1016/S0140-6736(20)32218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389:941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- 154.Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq. 1996;24:99–110. [Google Scholar]
- 155.Gilbert L, Raj A, Hien D, Stockman J, Terlikbayeva A, Wyatt G. Targeting the SAVA (substance abuse, violence and AIDS) syndemic among women and girls: a global review of epidemiology and integrated interventions. J Acquir Immune Defic Syndr. 2015;69(suppl 2):S118–S127. doi: 10.1097/QAI.0000000000000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26:392–407. doi: 10.3109/09540261.2014.928270. [DOI] [PubMed] [Google Scholar]
- 157.Niedzwiedz CL, Mitchell RJ, Shortt NK, Pearce JR. Social protection spending and inequalities in depressive symptoms across Europe. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1005–1014. doi: 10.1007/s00127-016-1223-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Reeves A, McKee M, Mackenbach J, Whitehead M, Stuckler D. Introduction of a national minimum wage reduced depressive symptoms in low-wage workers: a quasi-natural experiment in the UK. Health Econ. 2017;26:639–655. doi: 10.1002/hec.3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Venkataramani AS, Shah SJ, O'Brien R, Kawachi I, Tsai AC. Health consequences of the US Deferred Action for Childhood Arrivals (DACA) immigration programme: a quasi-experimental study. Lancet Public Health. 2017;2:e175–e181. doi: 10.1016/S2468-2667(17)30047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wahlbeck K, McDaid D. Actions to alleviate the mental health impact of the economic crisis. World Psychiatry. 2012;11:139–145. doi: 10.1002/j.2051-5545.2012.tb00114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Haushofer J, Shapiro J. The short-term impact of unconditional cash transfers to the poor: experimental evidence from Kenya. Q J Econ. 2016;131:1973–2042. doi: 10.1093/qje/qjw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Alves FJO, Machado DB, Barreto ML. Effect of the Brazilian cash transfer programme on suicide rates: a longitudinal analysis of the Brazilian municipalities. Soc Psychiatry Psychiatr Epidemiol. 2019;54:599–606. doi: 10.1007/s00127-018-1627-6. [DOI] [PubMed] [Google Scholar]
- 163.Angeles G, de Hoop J, Handa S, Kilburn K, Milazzo A, Peterman A. Government of Malawi's unconditional cash transfer improves youth mental health. Soc Sci Med. 2019;225:108–119. doi: 10.1016/j.socscimed.2019.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ohrnberger J, Fichera E, Sutton M, Anselmi L. The worse the better? Quantile treatment effects of a conditional cash transfer programme on mental health. Health Policy Plan. 2020;35:1137–1149. doi: 10.1093/heapol/czaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Shields-Zeeman L, Pathare S, Walters BH, Kapadia-Kundu N, Joag K. Promoting wellbeing and improving access to mental health care through community champions in rural India: the Atmiyata intervention approach. Int J Ment Health Syst. 2017;11:6. doi: 10.1186/s13033-016-0113-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Daruwalla N, Machchhar U, Pantvaidya S, et al. Community interventions to prevent violence against women and girls in informal settlements in Mumbai: the SNEHA-TARA pragmatic cluster randomised controlled trial. Trials. 2019;20:743. doi: 10.1186/s13063-019-3817-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Guzder J, Paisley V, Robertson-Hickling H, Hickling FW. Promoting resilience in high-risk children in Jamaica: a pilot study of a multimodal intervention. J Can Acad Child Adolesc Psychiatry. 2013;22:125–130. [PMC free article] [PubMed] [Google Scholar]
- 168.Ndetei DM, Mutiso V, Gitonga I, et al. World Health Organization life-skills training is efficacious in reducing youth self-report scores in primary school going children in Kenya. Early Interv Psychiatry. 2019;13:1146–1154. doi: 10.1111/eip.12745. [DOI] [PubMed] [Google Scholar]
- 169.Buller AM, Hidrobo M, Peterman A, Heise L. The way to a man's heart is through his stomach?: a mixed methods study on causal mechanisms through which cash and in-kind food transfers decreased intimate partner violence. BMC Public Health. 2016;16:488. doi: 10.1186/s12889-016-3129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Patel V, Burns JK, Dhingra M, Tarver L, Kohrt BA, Lund C. Income inequality and depression: a systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry. 2018;17:76–89. doi: 10.1002/wps.20492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Carey G, Crammond B, De Leeuw E. Towards health equity: a framework for the application of proportionate universalism. Int J Equity Health. 2015;14:81. doi: 10.1186/s12939-015-0207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Plagerson S, Patel V, Harpham T, Kielmann K, Mathee A. Does money matter for mental health? Evidence from the Child Support Grants in Johannesburg, South Africa. Glob Public Health. 2011;6:760–776. doi: 10.1080/17441692.2010.516267. [DOI] [PubMed] [Google Scholar]
- 173.Patz JA, Frumkin H, Holloway T, Vimont DJ, Haines A. Climate change: challenges and opportunities for global health. JAMA. 2014;312:1565–1580. doi: 10.1001/jama.2014.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Das P, Horton R. Disease Control Priorities, 3rd edition–from theory to practice. Lancet. 2018;391:e9–10. doi: 10.1016/S0140-6736(17)32905-7. [DOI] [PubMed] [Google Scholar]
- 175.Clinton W. Office of the UN Secretary-General's Special Envoy for Tsunami Recovery; New York, NY: 2006. Lessons learned from tsunami recovery: key propositions for building back better. [Google Scholar]
- 176.WHO . World Health Organization; Geneva: 2013. Building back better: sustainable mental health care after emergencies. [Google Scholar]
- 177.Maulik PK, Thornicroft G, Saxena S. Roadmap to strengthen global mental health systems to tackle the impact of the COVID-19 pandemic. Int J Ment Health Syst. 2020;14:57. doi: 10.1186/s13033-020-00393-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Patel V, Belkin GS, Chockalingam A, Cooper J, Saxena S, Unützer J. Grand challenges: integrating mental health services into priority health care platforms. PLoS Med. 2013;10 doi: 10.1371/journal.pmed.1001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: lessons from low-and middle-income countries. Annu Rev Clin Psychol. 2017;13:149–181. doi: 10.1146/annurev-clinpsy-032816-045217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Kohrt BA, Bhardwaj A. In: Global mental health and psychotherapy: adapting psychotherapy for low- and middle-income countries. Stein DJ, Bass JK, Hofmann SG, editors. Elsevier; London: 2019. Training and supervision; pp. 47–65. [Google Scholar]
- 181.Muke SS, Tugnawat D, Joshi U, et al. Digital training for non-specialist health workers to deliver a brief psychological treatment for depression in primary care in India: findings from a randomized pilot study. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17176368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Waters R. Community workers lend human connection to COVID-19 response. Health Aff (Millwood) 2020;39:1112–1117. doi: 10.1377/hlthaff.2020.00836. [DOI] [PubMed] [Google Scholar]
- 183.Sugiura K, Mahomed F, Saxena S, Patel V. An end to coercion: rights and decision-making in mental health care. Bull World Health Organ. 2020;98:52–58. doi: 10.2471/BLT.19.234906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiol Psychiatr Sci. 2016;25:113–122. doi: 10.1017/S2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Bellamy C, Schmutte T, Davidson L. An update on the growing evidence base for peer support. Ment Health Soc Inc. 2017;21:161–167. [Google Scholar]
- 186.Brown T, Wyatt J. Design thinking for social innovation. Development Outreach. 2010;12:29–43. [Google Scholar]
- 187.Bazzano AN, Martin J, Hicks E, Faughnan M, Murphy L. Human-centred design in global health: a scoping review of applications and contexts. PLoS One. 2017;12 doi: 10.1371/journal.pone.0186744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Thornicroft G, Ahuja S, Barber S, et al. Integrated care for people with long-term mental and physical health conditions in low-income and middle-income countries. Lancet Psychiatry. 2019;6:174–186. doi: 10.1016/S2215-0366(18)30298-0. [DOI] [PubMed] [Google Scholar]
- 189.Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387:2423–2478. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Chisholm D, Flisher AJ, Lund C, et al. Scale up services for mental disorders: a call for action. Lancet. 2007;370:1241–1252. doi: 10.1016/S0140-6736(07)61242-2. [DOI] [PubMed] [Google Scholar]
Uncited References
- 124.Selamu M, Asher L, Hanlon C, et al. Beyond the biomedical: community resources for mental health care in rural Ethiopia. PLoS One. 2015;10 doi: 10.1371/journal.pone.0126666. [DOI] [PMC free article] [PubMed] [Google Scholar]