Abstract
Background
A novel coronavirus disease (COVID-19) outbreak due to the severe respiratory syndrome coronavirus (SARS-CoV-2) infection occurred in China in late December 2019. Facemask wearing with proper hand hygiene is considered an effective measure to prevent SARS-CoV-2 transmission, but facemask wearing has become a social concern due to the global facemask shortage. China is the major facemask producer in the world, contributing to 50% of global production. However, a universal facemask wearing policy would put an enormous burden on the facemask supply.
Methods
We performed a policy review concerning facemasks using government websites and mathematical modelling shortage analyses based on data obtained from the National Health Commission (NHC), the Ministry of Industry and Information Technology (MIIT), the Centre for Disease Control and Prevention (CDC), and General Administration of Customs (GAC) of the People's Republic of China. Three scenarios with respect to wearing facemasks were considered: (1) a universal facemask wearing policy implementation in all regions of mainland China; (2) a universal facemask wearing policy implementation only in the epicentre (Hubei province, China); and (3) no implementation of a universal facemask wearing policy.
Findings
Regardless of different universal facemask wearing policy scenarios, facemask shortage would occur but eventually end during our prediction period (from 20 Jan 2020 to 30 Jun 2020). The duration of the facemask shortage described in the scenarios of a country-wide universal facemask wearing policy, a universal facemask wearing policy in the epicentre, and no universal facemask wearing policy were 132, seven, and four days, respectively. During the prediction period, the largest daily facemask shortages were predicted to be 589·5, 49·3, and 37·5 million in each of the three scenarios, respectively. In any scenario, an N95 mask shortage was predicted to occur on 24 January 2020 with a daily facemask shortage of 2·2 million.
Interpretation
Implementing a universal facemask wearing policy in the whole of China could lead to severe facemask shortage. Without effective public communication, a universal facemask wearing policy could result in societal panic and subsequently, increase the nationwide and worldwide demand for facemasks. These increased demands could cause a facemask shortage for healthcare workers and reduce the effectiveness of outbreak control in the affected regions, eventually leading to a pandemic. To fight novel infectious disease outbreaks, such as COVID-19, governments should monitor domestic facemask supplies and give priority to healthcare workers. The risk of asymptomatic transmission and facemask shortages should be carefully evaluated before introducing a universal facemask wearing policy in high-risk regions. Public health measures aimed at improving hand hygiene and effective public communication should be considered along with the facemask policy.
Keyword: Novel coronavirus-infected pneumonia, COVID-19, SARS-CoV-2, Facemask shortage, Public health intervention, Universal facemask wearing policy
Introduction
A large number of novel coronavirus disease (COVID-19) cases were initially identified in Wuhan, Hubei province, China in December 2019. The severe respiratory syndrome coronavirus (SARS-CoV-2) is mainly transmitted via respiratory droplets and can be transmitted between humans [1], [2], [3]. Common symptoms include fever, cough, dyspnoea, and myalgia/fatigue while less common symptoms include sputum production, headache, haemoptysis, and diarrhoea [4]. By 13 March 2020, the reported incidence of COVID-19 cases exceeded 80,000 in China of which more than 60% was in Wuhan city, and more than 80% was in Hubei province [5,6]. Globally, Thailand, Japan, South Korea, Singapore, Malaysia, France, Canada, Australia, Germany, the United Kingdom, the United States, and 111 other countries have reported COVID-19 cases.[7] Most of the confirmed cases were locally transmitted cases outside of China [7].
The World Health Organization's (WHO) guidelines concerning prevention and control of the COVID-19 outbreak recommends hand and respiratory hygiene and the use of appropriate personal protective equipment for healthcare workers in practice [8]. Patients with suspected SARS-CoV-2 infection should be offered a medical mask [8]. Regarding respiratory hygiene measures, facemask wearing with proper hand hygiene has been considered an effective measure to prevent COVID-19 transmission although WHO recommends against wearing facemasks in community settings [9,10]. Furthermore, the worldwide facemask shortage during the COVID-19 outbreak has become a social concern [11].
China is the major facemask producer in the world, contributing to 50% of the global production [12]. Normally, China can produce about 20 million facemasks per day while the productivity during the Chinese New Year holiday was lower (12 million facemasks per day) [12]. However, even if full productivity could be achieved, 20 million facemasks per day do not seem to meet the needs of a population of 1·4 billion in China under a universal facemask wearing policy. Therefore, to control the COVID-19 outbreak, the Chinese government imported more than 2·0 billion facemasks between 24 Jan 2020 and 29 Feb 2020 and extended the Chinese New Year holiday to allow for home quarantine in order to reduce the need for facemasks and other medical resources [13]. A number of factories also resumed partial productivity during the holiday by paying extra wages to their workers [14].
In this study, we simulated facemask availability during the COVID-19 outbreak using a mathematical model based on the actual development of the outbreak, public health measures introduced by the Chinese government, and national statistics on facemask production and import. We aimed to investigate the severity of the facemask shortage during the COVID-19 outbreak in China in different scenarios of facemask wearing policy and reflect on the effectiveness of this type of policy.
Methods
A cluster of COVID-19 cases was reported by the Wuhan Municipal Health Commission in late Dec 2019 [1]. The human-to-human transmission of COVID-19 was confirmed on 20 Jan 2020 by National Health Commission (NHC) of China [15]. The peak of the epidemic was estimated to be around 12 Mar 2020, and the epidemic in China has been predicted to end in late June [16,17]. The number of new cases is expected to decline after the epidemic peak, but viral transmission is still possible, and the need for facemasks will not decrease immediately. Therefore, our analysis covers the period from 20 Jan 2020 to 30 Jun 2020 (162 days in total). To simulate facemask availability in China, we used a mathematical model based on data and assumptions on the production, import, and need. Five user groups were taken into account: (1) healthcare workers; (2) infected inpatient cases, i.e., confirmed cases who are receiving treatment in hospitals; (3) suspected cases, i.e., people with respiratory symptoms; (4) observational cases, i.e., people with history of close contact with infected or suspected cases and are under medical observation; and (5) the general population. We assumed healthcare workers and infected inpatient cases need N95 facemasks while suspected and observational cases and the general population need non-N95 facemasks. We also assumed that when the N95 facemask shortage occurred, healthcare workers and infected inpatient cases would use non-N95 facemasks instead. We considered three scenarios of facemask wearing policy: (1) a universal facemask wearing policy was implemented in all regions of mainland China; (2) a universal facemask wearing policy was implemented only in the epicenter (Hubei province, China); and (3) no implementation of a universal facemask wearing policy. Universal facemask wearing policy refers to the recommendation of wearing facemasks in community settings [18].
Mathematical model
We simulated the daily facemasks availability using Eq. (1)
| (1) |
in which Fa(d) is facemask availability defined as the total number of facemasks on the market and in storage at the end of day d. Fa(0) (i.e., d = 0) is the baseline facemask availability at the beginning of our prediction period. Fp(d) is the number of facemasks produced in China on day d. Fi(d) is the number of facemasks imported to China on day d. Fn(d) is the need for facemasks on day d.
We estimated the daily need for facemasks using Eqs. (2)–(7)
| (2) |
| (3) |
| (4) |
| (5) |
| (6) |
| (7) |
in which Nn.h is the need for facemasks for healthcare worker while Fn.i(d), Fn.s(d), Fn.o(d) and Fn.g(d) indicate the need for facemasks for infected inpatient, suspected, and observational cases and the general population on day d, respectively. We set α(d) and θ as the need for facemasks for each healthcare workers on day d and the percentage of healthcare workers working on duty. We set β, γ, δ, and ε as the daily need for facemasks for each infected inpatient, suspected, and observational case, and each person among the general population, respectively. Ng and Nh are the numbers of the general population and healthcare workers, respectively. Ni(d), Ns(d), and No(d) are the numbers of infected inpatient, suspected, and observational cases on day d, respectively. Pg(d) is the percentage of the general population needing facemasks on day d.
Data source and model assumptions
Public health measures introduced by the Chinese government during the COVID-19 outbreak and the daily numbers of newly confirmed cases and deaths were summarized based on official announcements and documents from the National Health Commission (NHC), the Ministry of Industry and Information Technology (MIIT), the Centre for Disease Control and Prevention (CDC), and General Administration of Customs (GAC) of the People's Republic of China.
The parameters included in the mathematical model were estimated based on the data released by the NHC, MIIT, GAC, and CDC of the People's Republic of China or recent investigations concerning the outbreak. Model input and assumptions in our model are summarized in Table 1. Specifically, the population and numbers of active healthcare workers in mainland China and in Hubei province were obtained from China Health Statistics Yearbook 2019 [19]. We assumed that 80% of the healthcare workers would be on duty during any day of our prediction (θ). The numbers of infected inpatient, suspected, and observational cases between 20 Jan 2020 and 14 March 2020 were obtained from the NHC. Based on the clinical experience of chief physicians in China, we assumed the need for facemasks of each healthcare worker in Hubei province (α1(d)) and in other regions (α2(d)) on day d during our prediction period. We also assumed each infected inpatient, suspected, and observational case, and the general population would need five, two, two, and one facemask per day, respectively. We assumed that 50% of facemask consumption (σ1) consisted of N95 facemasks among healthcare workers in Hubei province and 10% (σ2) in other regions. We assumed that the percentages of general population wearing facemasks in Hubei province (Pg.h(d)) and in other regions of mainland China (Pg.o(d)) changed as the outbreak entered different stages. In our model, we assumed all facemasks on the market and in storage are available for consumption. In other words, we did not take into account factors that may limit the supply on the market, such as logistics.
Table 1.
Parameters for estimating the facemask availability during the novel coronavirus disease (COVID-19) outbreak in China.
| Parameter | Definition | Data source or assumptions | Model input |
|---|---|---|---|
| Ng.c | General population of mainland China | Data from China Health Statistics Yearbook 2019 | 1,395,380,000 |
| Ng.h | General population of Hubei province, China | Data from China Health Statistics Yearbook 2019 | 59,170,000 |
| Nh.c | Number of healthcare workers in mainland China | Data from China Health Statistics Yearbook 2019 | 12,300,325 |
| Nh.h | Number of healthcare workers in Hubei province | Data from China Health Statistics Yearbook 2019 | 521,930 |
| Nh.o | Number of healthcare workers in other regions | Data from China Health Statistics Yearbook 2019 | 11,778,395 |
| Ni(d) | Number of infected inpatient cases in mainland China on day d | Data from National Health Commission of the People 's Republic of China | Supplementary table S1 |
| Ns(d) | Number of suspected cases in mainland China on day d | Data from National Health Commission of the People 's Republic of China | Supplementary table S1 |
| No(d) | Number of medical observation cases in mainland China on day d | Data from National Health Commission of the People 's Republic of China | Supplementary table S1 |
| θ | Percentage of healthcare workers working on their positions | Assuming that 80% of total registered healthcare workers are working on their positions | 80% |
| α1(d) | Number of facemasks need of each healthcare worker in Hubei province each day | 20 Jan 2020: 2 Between 21 Jan 2020 and 12 Mar 2020 (China said peak of COVID-19 ended on 12 Mar): 10 Between 13 Mar 2020 and 30 June 2020 (Chinese medical expert predicted the end of COVID-19): 5 | 2 (d = 0) 10 (0<d ≤ 52) 5 (52<d ≤ 162) |
| α2(d) | Number of facemasks need of each healthcare worker in other regions each day | 20 Jan 2020: 2 Between 21 Jan 2020 and 12 Mar 2020 (China said peak of COVID-19 ended on 12 Mar): 5 Between 13 Mar 2020 and 30 June 2020 (Chinese medical expert predicted the end of COVID-19): 3 | 2 (d = 0) 5 (0<d ≤ 52) 3 (52<d ≤ 162) |
| σ1 | Percentage of N95 facemasks for all the consumption of facemasks by healthcare workers in Hubei province | Assuming that 50% facemasks for all the consumption of facemasks by healthcare workers in Hubei province | 50% |
| σ2 | Percentage of N95 facemasks for all the consumption of facemasks by healthcare workers in other regions in mainland China | Assuming that 10% N95 facemasks for all the consumption of facemasks by healthcare workers in other regions in mainland China | 10% |
| β | Number of facemasks need of each infected inpatient case each day | Assuming that each infected inpatient case would use five facemasks each day | 5 |
| γ | Number of facemasks need of each suspected case each day | Assuming that each suspected case would use two facemasks each day | 2 |
| δ | Number of facemasks need of each medical observation case each day | Assuming that each medical observation case would use two facemasks each day | 2 |
| ε | Number of facemasks need of each general population each day | Assuming that each general population would use one facemask each day | 1 |
| Pg.h(d) | Percentage of population in Hubei province using facemasks on day d | We assume the percentage of population using facemasks as following: Between 21 Jan 2020 and 23 Jan 2020: 40% (Last working day before Spring festival holiday on 23 Jan 2020) Between 24 Jan 2020 and 9 Feb 2020: 20% (Spring festival holiday ended on 9 Feb 2020 but general people in Hubei province were required to home quarantine) Between 10 Feb 2020 and 12 Mar 2020: 40% (China announced that the peak of COVID-19 ended on 12 Mar 2020) Between 13 Mar 2020 and 30 Apr 2020: 30% Between 1 May 2020 and 30 June 2020: 20% | 40% (0<d ≤ 3) 20% (3<d ≤ 20) 40% (20<d ≤ 52) 30% (52<d ≤ 101) 20% (101<d ≤ 162) |
| Pg.o(d) | Percentage of population in other regions of mainland China using facemasks on day d | We assume the percentage of population using facemasks as following: Between 21 Jan 2020 and 23 Jan 2020: 40% (Last working day before Spring festival holiday on 23 Jan 2020) Between 24 Jan 2020 and 9 Feb 2020: 20% (Spring festival holiday ended on 9 Feb 2020) Between 10 Feb 2020 and 12 Mar 2020: 40% (China announced that the peak of COVID-19 ended on 12 Mar 2020) Between 13 Mar 2020 and 31 Mar 2020: 30% Between 1 Apr 2020 and 30 Apr 2020: 20% Between 1 May 2020 and 31 May 2020: 10% Between 1 June 2020 and 30 June 2020: 5% | 40% (0<d ≤ 3) 20% (3<d ≤ 20) 40% (20<d ≤ 52) 30% (52<d ≤ 71) 20% (71<d ≤ 101) 10% (101<d ≤ 132) 5% (132<d ≤ 162) |
| Fp.N(d) | Number of N95 facemasks produced in China on day d | Estimation based on information from MIIT Between 21 Jan 2020 and 24 Jan 2020: 600,000 Between 25 Jan 2020 and 1 Feb 2020: 107,000 Between 2 Feb 2020 and 10 Feb 2020: 417,500 Between 11 Feb 2020 and 21 Feb 2020: 728,000 Between 22 Feb 2020 and 28 Feb 2020: 919,000 Between 29 Feb 2020 and 30 Jun 2020: 1660,000 | 600,000 (0<d ≤ 4) 107,000 (4<d ≤ 12) 417,500 (12<d ≤ 21) 728,000 (21<d ≤ 32) 919,000 (32<d ≤ 39) 1660,000 (39<d ≤ 162) |
| Fp(d) | Number of total facemasks produced in China on day d | Estimation based on information from MIIT Between 21 Jan 2019 and 24 Jan 2020: 20,000,000 Between 25 Jan 2020 and 2 Feb 2020: 8000,000 Between 3 Feb 2020 and 10 Feb 2020: 12,000,000 Between 11 Feb 2020 and 16 Feb 2020: 18,800,000 Between 17 Feb 2020 and 21 Feb 2020: 36,85,000 Between 22 Feb 2020 and 24 Feb 2020: 54,770,000 Between 25 Feb 2020 and 28 Feb 2020: 76,190,000 Between 29 Feb 2020 and 30 Jun 2020: 116,000,000 | 20,000,000 (0<d ≤ 4) 8000,000 (4<d ≤ 13) 12,000,000 (13<d ≤ 21) 18,800,000 (21<d ≤ 27) 36,785,000 (27<d ≤ 32) 54,770,000 (32<d ≤ 35) 76,190,000 (35<d ≤ 39) 116,000,000 (39<d ≤ 162) |
| Fi(d) | Number of total facemasks imported to China on day d | Estimation based on information from MIIT and GAC Between 24 Jan 2020 and 29 Jan 2020: 6000,000 30 Jan 2020: 20,000,000 Between 31 Jan 2020 and 11 Feb 2020: 56,166,667 Between 12 Feb 2020 and 24 Feb 2020: 83,384,615 Between 25 Feb 2020 and 29 Feb 2020: 40,000,000 Between 1 Mar 2020 and 5 Mar 2020: 20,000,000 Between 6 Mar 2020 and 10 Mar 2020: 10,000,000 Between 11 Mar 2020 and 15 Mar 2020: 5000,000 Between 16 Mar 2020 and 20 Mar 2020: 2500,000 Between 21 Mar 2020 and 30 Jun 2020: 0 | 6000,000 (4 ≤ d ≤ 9) 20,000,000 (d = 10) 56,166,667 (10<d ≤ 22) 83,384,615 (22<d ≤ 35) 40,000,000 (35<d ≤ 40) 20,000,000 (40<d ≤ 45) 10,000,000 (45<d ≤ 50) 5000,000 (50<d ≤ 55) 2500,000 (55<d ≤ 60) 0 (60<d ≤ 162) |
| Fi.N(d) | Number of N95 facemasks imported to China on day d | Assuming that 10% of import facemasks were N95 facemasks Fi.N(d)=10% × Fi(d) Between 24 Jan 2020 and 29 Jan 2020: 600,000 30 Jan 2020: 2000,000 Between 31 Jan 2020 and 11 Feb 2020: 5616,667 Between 12 Feb 2020 and 24 Feb 2020: 8338,462 Between 25 Feb 2020 and 29 Feb 2020: 4000,000 Between 1 Mar 2020 and 5 Mar 2020: 2000,000 Between 6 Mar 2020 and 10 Mar 2020: 1000,000 Between 11 Mar 2020 and 15 Mar 2020: 500,000 Between 16 Mar 2020 and 20 Mar 2020: 250,000 Between 21 Mar 2020 and 30 Jun 2020: 0 | 600,000 (4 ≤ d ≤ 9) 2000,000 (d = 10) 5616,667 (10<d ≤ 22) 8338,462 (22<d ≤ 35) 4000,000 (35<d ≤ 40) 2000,000 (40<d ≤ 45) 1000,000 (45<d ≤ 50) 500,000 (50<d ≤ 55) 250,000 (55<d ≤ 60) 0 (60<d ≤ 162) |
| Fa(0) | Number of facemasks available on 20 Jan 2020 | Facemask storage was estimated to be seven times the daily consumption in hospitals. We assume that 70% of the facemask storage in the whole of China would be supplied to the hospital system; thus, Fa(0) = 7 × (α1(0) × θ × Nh.h+ α2(0) × θ × Nh.o)/ 70% = 137,763,640 / 70% =196,805,200 | 196,805,200 |
| Fa.N(0) | Number of N95 facemasks available on 20 Jan 2020 | Assuming 10% of Number of facemasks available were N95 facemasks Fa.N(0)=10% × Fa(0)=19,680,520 | 19,680,520 |
MIIT estimated that China normally produces about 20 million facemasks daily. However, due to the Chinese New Year holiday and response to the outbreak, facemask productivity in early 2020 has experienced significant fluctuations. Therefore, we assumed that the daily N95 and total facemask productivity, Fp.N(d) and Fp(d), respectively, changed during our prediction period. According to the MIIT and GAC, China imported 2·0 billion facemasks between 24 Jan 2020 and 29 Feb 2020. The import volume in from March 2020 to the end of June was estimated based on the most recent report. We assumed that 10% of total import of facemasks were N95 facemasks. Facemask storage was estimated to be seven times the daily consumption found in hospitals [12]. We assume that 70% of the facemask storage in the whole of China would be supplied to the hospital system; thus, the baseline facemask availability, Fa(0) was estimated to be 196,805,200 (assuming N95 facemasks account for 10% of total facemask storage), which was about ten times the usual daily facemask productivity in China.
Results
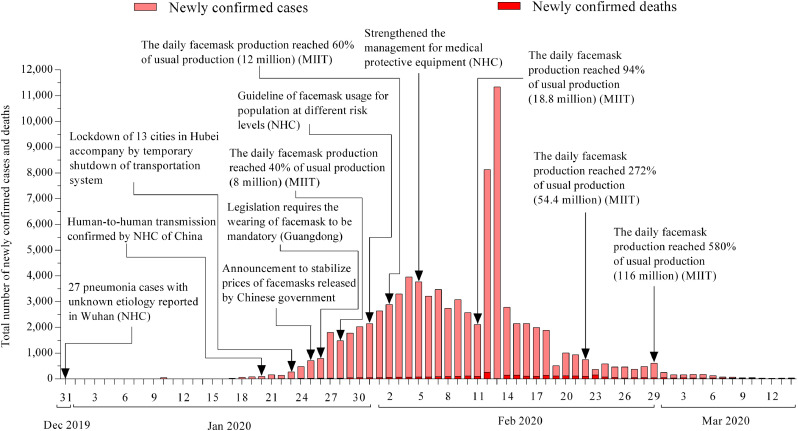
Fig. 1 shows the numbers of newly confirmed COVID-19 cases and deaths, public health interventions introduced by the Chinese government, and changes in facemask productivity from 31 Dec 2019 to 29 Feb 2020. The sharp increase in newly confirmed cases on 12 and 13 Feb 2020 was due to the release of the fifth version of the COVID-19 protocol in which “clinical diagnosis” was added into the diagnostic criteria of COVID-19 in Hubei province [20]. From the start of the Chinese spring festival holiday on 24 Jan 2020 until festival completion on 29 Feb 2020, daily facemask productivity increased from 8 to 116 million.
Fig. 1.
Daily new confirmed cases and deaths during the novel coronavirus disease (COVID-19) outbreak in China. (Publicly available data from official websites of the National Health Commission (NHC), the Ministry of Industry and Information Technology (MIIT), the center for Disease Control and Prevention (CDC), and General Administration of Customs (GAC) of the People's Republic of China).
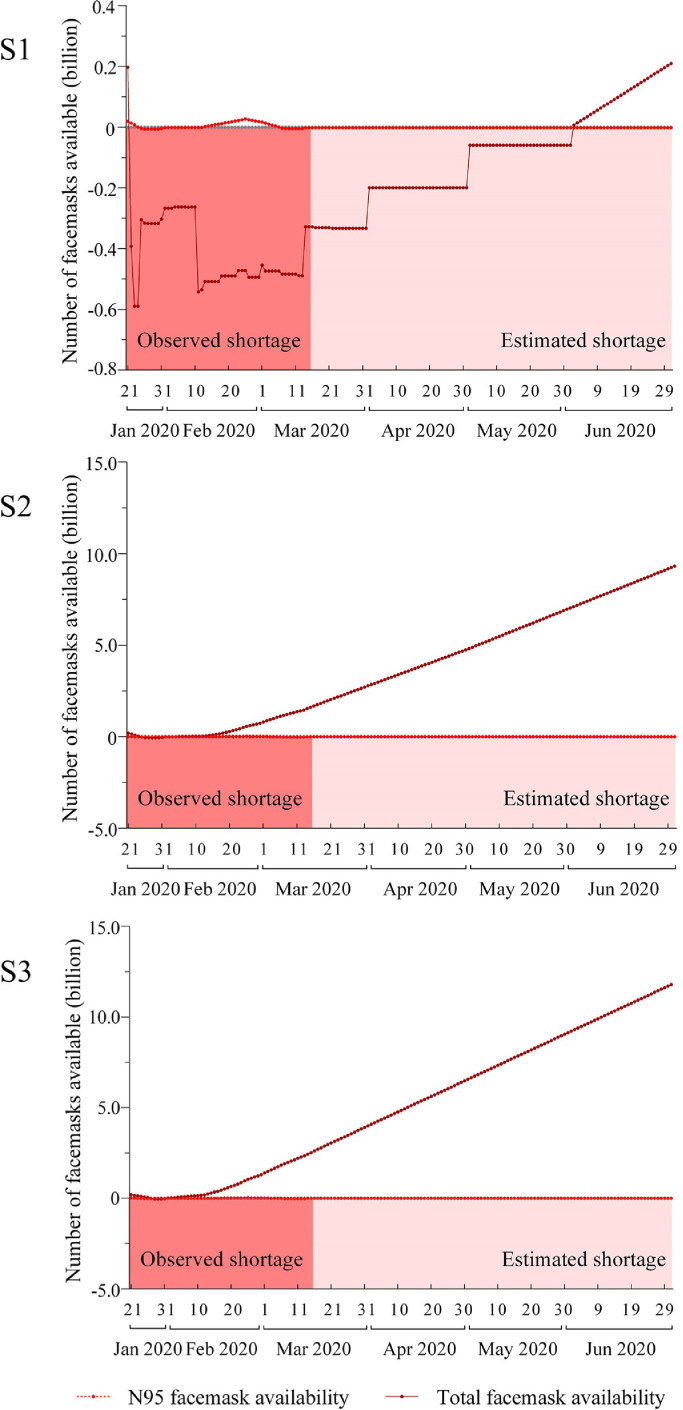
Fig. 2 shows the observed shortage and our prediction of the facemask availability (total and N95 facemasks) during the COVID-19 outbreak under different scenarios on the implementation of universal facemask wearing policy. Panic-buying and facemask price surges were reported on 20 Jan 2020 right after the confirmation of human-to-human transmission [21]. The Chinese government introduced price controls for facemasks on 25 Jan 2020 [22]. This observation indicated a facemask shortage starting as early as 20 Jan 2020, and there is no clear evidence showing the shortage has been relieved at the time of this analysis (14 Mar 2020). Our prediction model estimated the severity of the shortage between 20 Jan 2020 and 30 Jun 2020. In all of the facemask wearing policy scenarios, the shortage of N95 facemasks would occur on day 4 (24 Jan 2020) and last until the end of our prediction period (with a 2·2 million shortage), except for the period from 12 Feb 2020 to 5 Mar 2020. Specifically, in Scenario 1, assuming the universal facemask wearing policy was implemented in the whole of China, 392·6 million facemasks would have been in short supply on day 1 (21 Jan 2020), and the shortage would end on day 132 (31 May 2020). In Scenario 2, assuming a universal facemask wearing policy was implemented in Hubei province (the epicenter), 5·3 million facemasks would have been in short supply on day 4 (24 Jan 2020), and the shortage would end on day 10 (30 Jan 2020). In Scenario 3, assuming a universal facemask wearing policy was not implemented at all, 34·6 million facemasks were in short supply on day 7 (27 Jan 2020), and the shortage would end on day 10 (30 Jan 2020). During the prediction period, the maximum daily shortages of facemasks were 589·5, 49·3, and 37·5 million in each of the three scenarios, respectively.
Fig. 2.
Facemask availability during the novel coronavirus disease (COVID-19) outbreak in China (S1: assuming a universal facemask wearing policy implementation in all regions of mainland China; S2: assuming a universal facemask wearing policy implementation only in the epicenter (Hubei province, China); S3: Assuming no implementation of a universal facemask wearing policy).
Discussion
In this study, we summarized the public health measures introduced by the Chinese government to relieve the facemask shortage observed during the COVID-19 outbreak and simulated the facemask availability in three scenarios of facemask wearing policy to estimate the severity of the shortage. Our findings suggest that a facemask shortage, particularly for N95 facemasks, would occur regardless of the implementation of a universal facemask wearing policy. However, the facemask shortage could be much more severe if a universal facemask wearing policy was implemented in the whole of China rather than the most severely affected areas. In addition, the shortage of N95 facemask were not alleviated under the existing public health measures.
Facemasks, especially N95 facemasks, are essential protective equipment for healthcare workers during an infectious disease outbreak [8]. Confirmed infected and suspected cases are also recommended to wear a facemask to minimize virus transmission [10]. Numerous studies have reported the effects of wearing facemasks on restricting virus transmission, such as a 3–4-fold decrease in aerosol-associated viruses and lower transmission rate among their close contacts [23,24]. Thus, maintaining a stable supply of facemasks (especially N95 facemasks) with a priority given to healthcare workers and infected people is crucial for outbreak control [25,26]. In some East Asian regions, wearing a facemask in public during flu seasons and disease outbreaks is considered a measure to constrain asymptomatic transmission in the community settings and a social responsibility norm for outbreak control, particularly after the experience of the Severe Acute Respiratory Syndrome (SARS) in 2003 [27]. However, universal facemask wearing was not recommended by WHO [28]. Previous studies found that wearing facemasks may be effective only when combined with hand hygiene, and this combined measure could reduce exposure to aerosolized influenza virus by 6-fold [18,28,29]. Therefore, to reduce transmission of respiratory viruses, a combination of public health measures is needed, for example, frequent hand-washing, wearing masks and gloves, and isolation for infected and suspected cases [9].
During the COVID-19 outbreak, in addition to the universal facemask policy, the Chinese government introduced various measures, such as lockdown of cities, shutdown of the transportation system, school closure, and hand hygiene recommendations [26,[30], [31], [32]]. However, implementation of these responses was not always timely, and the virus eventually spread throughout the entire country. As soon as the general population began to realize the severity of the outbreak, facemask consumption surged in only a few days, partly due to the lack of information concerning the novel virus and panic buying [18]. Under these circumstances, the Chinese government made several attempts at various efforts with respect to public communication, including updating data concerning the latest facemask productivity, release of guidelines on facemask usage, stabilizing facemask prices on the market, and offering a facemask lottery in official pathways. NHC classified each province unit into different risk levels (high-, middle-, and low-risk) and implemented corresponding strategies for outbreak control on 27 Feb 2020 [33]. This strategy was similar to Scenario 2 in our analysis (universal facemask wearing policy implemented in the epicenter/high-risk region). The experience in China during the COVID-19 outbreak shows that a universal facemask wearing policy should be introduced with caution. In addition, both Hong Kong (with universal facemask wearing) and Singapore (without universal facemask wearing) experienced a slow increase in the number of new cases, indicating that a universal facemask wearing policy may not be necessary for outbreak control [34]. Given that the demand for facemasks can increase dramatically due to panic-buying, a universal facemask wearing policy in high-risk regions may be more appropriate to prevent massive asymptomatic infection. However, without effective public communication, a universal facemask wearing policy, even in specific regions, can result in panic throughout society and subsequently, increase the nationwide and worldwide demands for facemasks. These increased demands could cause a facemask shortage for healthcare workers and reduce the effectiveness of outbreak control in the affected regions, eventually leading to a pandemic.
To the best of our knowledge, this is the first study to investigate the facemask availability during the COVID-19 outbreak in China. We provided a detailed summary of the public health measures introduced by the Chinese government concerning facemasks and considered three facemask wearing policy scenarios. Nevertheless, there are some limitations in this study. First, our estimation relied on the assumptions of facemask productivity, import, storage, and need. Relevant information was limited at the time that the analyses were performed (during the epidemic). Second, we did not consider logistics cost that could restrict facemask supplies on the markets. Thus, our analysis is likely to underestimate the severity of the facemask shortage experienced by the healthcare workers and other user groups. Third, our prediction ended in late June considering the epidemic has been predicted to fade out by that time [17]. However, if imported infected cases cannot be controlled, the end of the epidemic will be delayed; thus, the daily incidence and facemask demand will also increase. Nevertheless, the anxiety in the population may result in constant demands for facemasks even when the epidemic is under controlled.
Implementing a universal facemask wearing policy in the whole of China could lead to severe facemask shortage. Although a universal facemask wearing policy in high-risk regions may be considered in order to prevent massive asymptomatic infection, nationwide or even worldwide facemask shortage is likely to occurred without effective public communication. Facemask shortage for healthcare workers would restrict the effectiveness of outbreak control in the affected regions and eventually lead to a pandemic. To fight novel infectious disease outbreaks, such as COVID-19, governments should monitor domestic facemask supplies and give priority to healthcare workers. Risk of asymptomatic transmission and facemask supply and demand should be carefully evaluated before introducing a universal facemask wearing policy in high-risk regions. Public health measures aimed at improving hand hygiene and effective public communication should be considered along with facemask wearing policy.
Declaration of Competing Interest
No conflicts of interest.
Data sharing statement
All data used in this study are publicly available. Data sources are described in the method section.
Role of funding
No funding in this study.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2020.100329.
Contributor Information
Huai-liang Wu, Email: wuhuailiang@stu2014.jnu.edu.cn.
Jian Huang, Email: jian.huang@imperial.ac.uk.
Casper J.P. Zhang, Email: casperz1@connect.hku.hk.
Zonglin He, Email: hezonglin0leon@stu2015.jnu.edu.cn.
Wai-Kit Ming, Email: wkming@connect.hku.hk.
Appendix. Supplementary materials
Reference
- 1.Nishiura H., Jung S.M., Linton N.M. The extent of transmission of novel coronavirus in Wuhan, China, 2020. J Clin Med. 2020;9(2):330. doi: 10.3390/jcm9020330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P. Early transmission dynamics in wuhan, china, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. https://www.nejm.org/doi/full/10.1056/NEJMoa2001316#article_citing_articles [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cui J., Li F., Shi Z.L. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Health Commission of the People 's Republic of China . 2020. Updates on pneumonia of new coronavirus infections as of march 13, 2020 (in Chinese)http://www.nhc.gov.cn/xcs/yqfkdt/202003/ec0119a5881543288efd5b5c8008387b.shtml (accessed 14 Mar 2020) [Google Scholar]
- 6.Wuhan Municipal Health Commission . 2020. Wuhan municipal health commission briefing on the pneumonia epidemic situation, 13 march 2020 (in Chinese)http://wjw.wuhan.gov.cn/front/web/showDetail/2020031410102 (accessed 14 Mar 2020) [Google Scholar]
- 7.World Health Organization . 2020. Novel coronavirus (2019-nCoV) situation report - 53, 2020.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200313-sitrep-53-covid-19.pdf (accessed 14 Mar 2020) [Google Scholar]
- 8.World Health Organization . 2020. Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected.https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 (accessed 7 Feb 2020) [Google Scholar]
- 9.Jefferson T., Del Mar C., Dooley L. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. 2009;339:b3675. doi: 10.1136/bmj.b3675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization (WHO) 2020. Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (2019-nCoV)outbreak: interim guidance, 29 January 2020.https://apps.who.int/iris/handle/10665/330987 (accessed 13 Mar 2020) [Google Scholar]
- 11.World Health Organization (WHO) 2020. Shortage of personal protective equipment endangering health workers worldwide.https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed 8 Mar 2020) [Google Scholar]
- 12.Ministry of Industry and Information Technology of People's Republic of China . 2020. Facemasks shortage? Just now, the ministry of industry and information technology of people 's republic of China responded (in Chinese)http://www.miit.gov.cn/n973401/n7647394/n7647409/c7656383/content.html (accessed 7 Feb 2020) [Google Scholar]
- 13.2020. General administration of customs (GAC) of People 's Republic of China interpretation of Chinese foreign trade in previous two months (in Chinese)http://www.customs.gov.cn//customs/xwfb34/302425/2879133/index.html (accessed 15 Mar 2020) [Google Scholar]
- 14.Ministry of Industry and Information Technology of People 's Republic of China . 2020. A large numbers of clothing enterprises changed to produce facemasks and protective clothes (in Chinese)http://www.miit.gov.cn/n973401/n7647394/n7647409/c7675791/content.html (accessed 14 Feb 2020) [Google Scholar]
- 15.China Daily . 2020. Expert: people can transmit virus to others.https://epaper.chinadaily.com.cn/a/202001/21/WS5e263938a310a2fabb7a1ae1.html (accessed 15 Mar 2020) [Google Scholar]
- 16.Xinhua News Agency . 2020. China says its COVID-19 peak is over.http://www.xinhuanet.com/english/2020-03/12/c_138870547.htm (accessed 12 Mar 2020) [Google Scholar]
- 17.Xinhua News Agency . 2020. Update: expert says global COVID-19 could be controlled "by June" if most countries act like China.http://www.xinhuanet.com/english/2020-03/12/c_138870768.htm (accessed 12 Mar 2020) [Google Scholar]
- 18.Leung C.C., Lam T.H., Cheng K.K. Mass masking in the COVID-19 epidemic: people need guidance. Lancet. 2020 doi: 10.1016/S0140-6736(20)30520-1. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30520-1/fulltext [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Health Commission of the People 's Republic of China . 2019. Chinese health statistics yearbook (2019 version) (in Chinese) China. [Google Scholar]
- 20.National Health Commission of the People 's Republic of China (NHC) 2020. The protocol for the novel coronavirus pneumonia (the fifth version) (in Chinese)http://www.nhc.gov.cn/yzygj/s7653p/202002/d4b895337e19445f8d728fcaf1e3e13a.shtml (accessed 11 Mar 2020) [Google Scholar]
- 21.CCTV.com . 2020. How to promise the stabilization of prices of facemask supplies and allow general population to have sense of security? (in Chinese)http://news.cctv.com/2020/01/23/ARTIWF9PRGr0wnnxC1pDha3G200123.shtml (accessed 15 Mar 2020) [Google Scholar]
- 22.State Administration for Market Regulation of People 's Republic of China . 2020. Announcement of maintainance of medical protective equipment released by the state administration for market regulation (in Chinese)http://gkml.samr.gov.cn/nsjg/jjjzj/202001/t20200125_310740.html (accessed 15 Mar 2020) [Google Scholar]
- 23.Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9(3) doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sung A.D., Sung J.A.M., Thomas S. Universal mask usage for reduction of respiratory viral infections after stem cell transplant: a prospective trial. Clin Infect Dis. 2016;63(8):999–1006. doi: 10.1093/cid/ciw451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Industry and Information Technology of People 's Republic of China . 2020. Chinese medical N95 mask daily productivity is only 600,000! Forward the appeal, please leave it to the medical staff (in Chinese)http://www.miit.gov.cn/n973401/n7647394/n7647409/c7663732/content.html (accessed 7 Feb 2020) [Google Scholar]
- 26.National Health Commission of the People 's Republic of China . 2020. The announcement of publishing the guidelines of protection of population at different risk levels for novel coronavirus and facemasks usage to prevent the novel coronavirus infection (in Chinese)http://www.nhc.gov.cn/jkj/s7916/202001/a3a261dabfcf4c3fa365d4eb07ddab34.shtml (accessed 7 Feb 2020) [Google Scholar]
- 27.The Government of the Hong Kong Special Administrative Region . 2020. Health advice of COVID-19. (accessed 15 Mar 2020) [Google Scholar]
- 28.World Health Organization (WHO) 2020. Coronavirus disease (COVID-19) advice for the public: when and how to use masks.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks (accessed 12 Mar 2020) [Google Scholar]
- 29.Makison Booth C., Clayton M., Crook B., Gawn J.M. Effectiveness of surgical masks against influenza bioaerosols. J Hosp Infect. 2013;84(1):22–26. doi: 10.1016/j.jhin.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 30.Chinese Center for Disease Control and Prevention (CDC) 2020. Chinese center for disease control and prevention (CDC) tips of prevention for COVID-19.http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_2275/202003/t20200308_214205.html (accessed 15 Mar 2020) [Google Scholar]
- 31.World Heath Organization . 2020. WHO, China leaders discuss next steps in battle against coronavirus outbreak.https://www.who.int/news-room/detail/28-01-2020-who-china-leaders-discuss-next-steps-in-battle-against-coronavirus-outbreak (accessed 7 Feb 2020) [Google Scholar]
- 32.The Lancet COVID-19: too little, too late? Lancet. 2020;395(10226):755. doi: 10.1016/S0140-6736(20)30522-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Health Commission of the People 's Republic of China . 2020. To further implement scientific precious management strategies to provide medical management works during this COVID-19 outbreak (in Chinese)http://www.nhc.gov.cn/yzygj/s7659/202002/76a2bd9a66e145339d2552211891c0f0.shtml (accessed 11 Mar 2020) [Google Scholar]
- 34.World Health Organization (WHO) 2020. Coronavirus disease (COVID-2019) situation reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed 15 Mar 2020) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.