Abstract
In this study, we introduce the ‘racial opportunity gap’ as a place-based measure of structural racism for use in population health research. We first detail constructing the opportunity gap using race-sex specific estimates of intergenerational economic mobility outcomes for a recent cohort. We then illustrate its utility in examining spatial variation in the racial mortality gap. First we demonstrate a correlation between the racial opportunity gap and the racial mortality gap across U.S. counties; where the gap in the adult earnings of black and white children born to families at the same income level is greater so, too, is the gap in mortality. Second, we show in a multivariable framework that the racial opportunity gap is associated with the racial mortality gap net of differences in the socioeconomic composition of the two groups. In so doing, we aim to provide population health researchers with a new empirical tool and analytic framework for examining the role of structural racism in generating racial health disparities.
Keywords: Race, Racism, Mortality, Racial health disparities, Population health, Inequality
Racial disparities in health persist despite advances in public health, medical technology and expanded access to health care (Hummer, 1996). Despite evidence of narrowing in recent years (Cunningham et al., 2017), the racial mortality gap remains large, with life expectancies for black males and black females 4.4 years and 2.9 years lower than their white counterparts (NCHS 2018). Notably, the size of the racial mortality gap varies substantially across U.S. localities. This spatial variation has motivated a fast-growing literature examining how structural features of place shape racial health disparities (see, e.g., Cullen, Cummins, & Fuchs, 2012; Browning, Cagney, & Ming, 2003; Gebreab & Diez Roux, 2012), one component of a broader push across the social sciences to consider theoretically and empirically how racism impacts population health (Hardeman et al 2016, 2018).
Williams and Collins (1995; 2015) identify structural racism as one of three broad categories—alongside cultural racism and individual-level discrimination—of pathways through which racism generates racial health disparities. This 3-tier categorization highlights that racism operates through a cultural ideological environment of inferiority that undergirds discriminatory behaviors enacted by individuals and informal groups, as well as at the macro-level via formal rules and procedures of social and political institutions, known as institutional racism (Carmichael & Hamilton, 1967; Williams et al., 2019). Theories of institutional racism give preeminence to racism that is embedded within normed and often overlooked policies and practices of organizations and structures, and structural racism expands upon this perspective to consider how the interactions among institutions produce racialized outcomes (Bailey, Krieger, Agénor, Graves, & Bassett, 2017; Williams and Collins., 1995; Williams et al., 2019). Under this conceptualization, structural racism then refers to interconnected institutions—such as housing, education, employment and earnings, credit, health care, political participation and the criminal justice system—whose linkages are both historically rooted and culturally maintained (Bailey et al., 2017).
Scholars from across the social sciences have endeavored to measure and isolate the effect of these different forms of racism on population health. Innovative measures of perceived discrimination, for example, have been developed (Landrine & Klonoff, 1996; McNeilly et al., 1996; Williams et al. 1997, 2008) and applied to demonstrate the effect of individual level racism on a wide array of health outcomes (see Lewis, Cogburn, & Williams, 2015 for a review). Structural racism has proven harder to measure directly (Gee & Ford, 2011; Krieger, 2012). This research typically focuses on how particular features of a given ‘place’-–which varies from a city block to a neighborhood to a county or state depending on the social process of interest—map on to observed racial health disparities. This includes research on the racialized health effects of residential segregation (e.g., Kershaw et al., 2011; Mendez, Hogan, & Culhane, 2011; Williams & Collins, 2001), policy context (e.g., Chambers et al. 2018; Lukachko, Hatzenbuehler, & Keyes, 2014), local political economy (e.g., Sewell, 2016), incarceration (e.g., Nosrati et al. 2017; Wildeman & Wang, 2017) or even police killings (Bor, Venkataramani, Williams, & Tsai, 2018).
Other studies have pointed to ‘residual’ differences in the health outcomes of blacks and whites after accounting for individual-level SES differences as evidence of racism (see Phelan & Link, 2015 for a discussion; Geruso, 2012). Yet measuring the effect of place on health is complicated by the fact that race-based differences in SES and health are driven by the same ‘underlying process’ (Phelan & Link, 2015; Williams & Collins, 1995; Williams and Mohammed, 2013). This underlying process cannot be revealed by statistically adjusting for differences in SES composition; doing so “artificially creates equality in both the exposure and the outcome along the dimensions of race, obscuring potentially meaningful information about the mechanisms underpinning health inequities” ([173] Nuru-Jeter et al., 2018). Using SES disparities to account for health disparities serves to obscure the effect of place-based structural racism in generating both.
Why? Consider two hypothetical counties: County A and County B. Imagine at time 1 that the black and white populations of County A and County B are identical in every way: same levels of poverty, median income, educational attainment, etc. Now imagine we observe both counties again at time 2 and find that while the black and white populations in County A remain identical on all SES measures, the black and white populations in County B have diverged, with the black population posting higher levels of poverty and lower levels of income and education than the white population. This would lead us to conclude that the structural features of County B are interacting with race to generate racial disparities in SES outcomes but not so in County A. In this scenario, we can readily attribute observed racial differences in SES outcomes to structural differences in the place—operating through some combination of differences in school quality, neighborhood context, criminal justice practices, employment opportunities, and other factors. Having started with identical populations in time 1, the level of racial disparity observed in time 2 can be readily taken as a measure of the degree of structural racism.
Of course, in no place or time are the SES levels of black and white populations perfectly equal. Spatial differences in the SES composition of black and white populations are historically conditioned. That the poverty rate for blacks is higher than whites in a given place and time is the result of many disparate processes operating over generations, from patterns of migration and settlement to legacies of discrimination and exclusion to industry mix, business cycle dynamics and policy environment. These historically embedded, structural determinants of a place serve to influence life course trajectories in both socioeconomic status attainment and health. Given these processes work over the life course and across generations, racial differences in socioeconomic composition, e.g., differential poverty rates between blacks and whites, at a given moment does not necessarily capture the contemporaneous effect of place in generating racial disparities.
In this study, we introduce and motivate the ‘racial opportunity gap’ as a novel place-based measure of structural racism. The racial opportunity gap captures the difference in the adult earnings of black and white children born to families at the same income level. Specifically, the opportunity gap measures the difference in the income percentile ranking in adulthood between black and white children who started at the same place in the national income distribution. Conditional on being from families at the same income level, the extent to which black boys and girls fall economically behind their white peers in early adulthood reveals how race interacts with place to shape life chances. Where the racial opportunity gap is higher, so too is structural racism.
Critically, place-based differences in the size of the opportunity gap and the size of SES gaps vary independently. The racial opportunity gap can be low where gaps in SES are high and, conversely, the racial opportunity gap between blacks and whites can be high where differences in SES are low. In comparing the mobility outcomes of black and white children born to families in the same county at the same income percentile, the racial opportunity gap provides a direct summary measure of the effect of place in generating racial disparities in socioeconomic outcomes, regardless of the current level of SES disparities. The racial opportunity gap therefore offers a measure of the effect of place in generating racial SES disparities that does not conflate the size of black white differences in SES levels with the degree of structural racism in a place. The aim of our study is to examine whether this measure of structural racism can help us account for spatial patterns in racial health disparities, operationalized below using the racial mortality gap.
Data & analytic approach
Racial Opportunity Gap: We operationalize the racial opportunity gap as the difference in the intergenerational economic mobility outcomes of black and white children born to families at the same level of income in the same county. We construct this measure using race-sex-specific estimates of absolute economic mobility generated and made publicly available by Chetty, Hendren, Jones, and Porter (2018) from linked IRS administrative earnings records for a recent cohort of young adults and their parents measured decades earlier. Specifically, we take the difference in the average national income percentile ranking in adulthood achieved between white and black individuals in the same county born to parents at the 25th percentile of the national income distribution.
To illustrate: In Norfolk, VA, black boys born to families at the 25th income percentile move up on average to the 29th income percentile in adulthood; by comparison, white boys in Norfolk born to families at the 25th income percentile move up on average to the 39th income percentile in adulthood, amounting to a racial opportunity gap of 10 points.
We construct this measure (a) for each county and (b) separately for males and females, as Chetty and colleagues identified significant heterogeneity in the mobility experiences of black males and females both within and between places. This is consistent with an intersectional framework which considers how social structure presents unique and excess risks to individuals with multiple forms of social disadvantage—here race and sex—that are greater than the sum of each individual risk (see, e.g., Bauer, 2014; Richardson & Brown, 2016; Brown, RichardsonHargrove, & Thomas, 2016) as well as extant literature detailing differential mortality patterns for men and women (Crimmins, Shim, Zhang, & Kim, 2019).
Table 1 presents descriptive statistics for the racial opportunity gap. The mean (unweighted) gap across counties in our sample is 11 points for men and 10 points for women. White boys and girls achieve greater mobility outcomes than black boys and girls at the same level of family income in almost—but not quite—every county; the size of the racial opportunity gap at even the 10th percentile is substantively large, indicating that white girls and boys climb 6 and 7 percentile points higher in the income distribution than their black counterparts. Supplementary Table S1 presents results from OLS models estimating the size of the racial opportunity gap as a function of county level characteristics. Here we see the opportunity gap appears to be larger in the northeastern states and in counties with higher income inequality and a higher fraction of nonwhite residents whereas the gap is smaller in counties with greater population density and higher unemployment.
Table 1.
Descriptive statistics for the racial opportunity gap.
| Male (n= 1535) | Female (n= 1519) | |
|---|---|---|
| Mean | 11.23 | 10.32 |
| Median | 11.40 | 10.27 |
| Std. Dev. | 4.53 | 4.30 |
| Min | −15.17 | −13.52 |
| Max | 35.50 | 28.59 |
| 10th percentile | 5.98 | 5.33 |
| 90th percentile | 16.22 | 15.47 |
Note: Data for calculating the racial opportunity gap are publicly available from https://opportunityinsights.org/data/.
Racial Mortality Gap: We operationalize the racial mortality gap as the difference in age-adjusted all-cause mortality rates for non-Hispanic blacks and whites. We first draw on death records from the restricted-use multiple cause of death file from the National Center for Health Statistics and the Centers for Disease Control and Prevention to calculate age-adjusted, all-cause, race-sex-specific mortality rates. These mortality rates are age-adjusted using the year 2000 Standard Population. Since we focus on county-level opportunity gaps, we account for small cell sizes by pooling 5-years of death records and population counts, centered on the year 2015 (2013–2017). We use bridged-race population estimates from the NCHS as our denominators for calculating mortality rates. Upon calculating race-sex-specific mortality rates, we construct our racial mortality gap measure by taking the within-sex difference in age adjusted mortality rates.
Racial Gaps in Economic Outcomes: We construct race-sex specific gaps in socioeconomic outcomes at the county level using data from the American Community Survey (ACS) 5-year pooled sample 2013–2017. Consistent with the literature on mortality, we focus on within-sex race differences in poverty, unemployment, median income, and education (proportion college graduates). Descriptive statistics are presented in Table 2.
Table 2.
Descriptive statistics using both total (black + white) and black only population weights.
| Weights: | Males | Females | ||||||
|---|---|---|---|---|---|---|---|---|
| Total Male Pop | Black Male Pop | Total Female Pop | Black Female Pop | |||||
| Mean | S.D. | Mean | S.D. | Mean | S.D. | Mean | S.D. | |
| Mortality Gap (B–W) | 152.5 | 202.8 | 182.0 | 173.3 | 90.8 | 163.1 | 90.7 | 105.6 |
| Unemployment Gap (B–W) | 6.7 | 5.1 | 7.8 | 4.4 | 5.3 | 4.6 | 5.9 | 3.6 |
| Poverty Gap (B–W) | 17.4 | 10.2 | 18.6 | 9.1 | 20.3 | 12.2 | 20.5 | 9.7 |
| Median Income Gap (W–B) | 18.8 | 8.9 | 19.6 | 8.9 | 7.3 | 6.2 | 8.4 | 5.9 |
| B.A. or Greater Gap (W–B) | 18.0 | 11.0 | 21.7 | 11.4 | 13.4 | 11.5 | 16.5 | 11.9 |
| Opportunity Gap (W–B) | 12.5 | 3.8 | 13.2 | 3.3 | 11.1 | 3.8 | 11.8 | 3.6 |
| Counties | 1535 | 1519 | ||||||
Analytic Strategy: After listwise deletion, our female analytic sample contains 1519 counties covering 98.3% of the U.S. black female population and our male analytic sample contains 1535 counties covering 99% of the U.S. black male populations. We use OLS models to estimate the association between the racial opportunity gap and racial mortality gap across U.S. counties, separately for males and females. As many counties with a large total population have a numerically small black population, we present results for each model using two different (sex-specific) weighting schemas: the total (black and white) population and the black only population. As an empirical consideration, use of total population will analytically upweight many counties with imprecise mortality and SES measures for blacks given the small sample size. Moreover, our theoretical interest in structural racism motivates estimating models that analytically weight counties according to the size of the black population.
Results
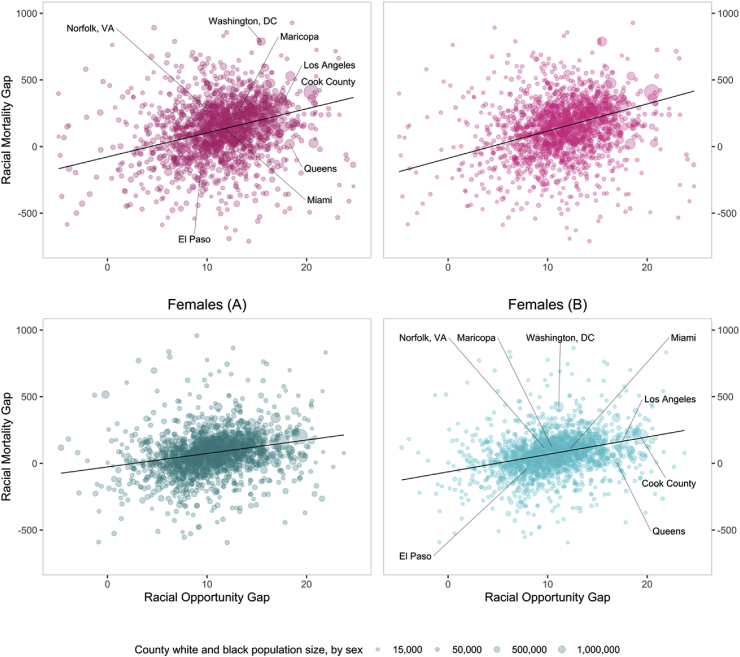
Fig. 1 plots the bivariate relationship between the racial opportunity gap (X-axis) and the racial mortality gap (Y-axis) separately for males (top) and females (bottom). Each dot represents a county and is scaled to either the size of the total (black + white) population weights (A) or the size of the black only population (B).
Fig. 1.
Racial mortality gap and racial opportunity gap across U.S. Counties total population weights (A) and black only population weights (B).
As expected, the size of the racial opportunity gap is positively associated with the size of the racial mortality gap across U.S. counties. Examining the figures weighted by total population (A), for males the slope coefficient on the fitted line indicates that moving from the 25th percentile of the racial opportunity gap (8.80) to the 75th percentile (14.02) is associated with an 85 deaths per 100,000 increase in the racial mortality gap. For females the association is a bit weaker, with a move from the 25th percentile of the racial opportunity gap (7.86) to the 75th percentile (12.86) associated with an increase in the racial mortality gap of about 50 deaths per 100,000. Notably, the fitted lines are slightly steeper for both men and women when weighting counties by the size of the black only population.Where the racial opportunity gap is higher so too is the racial mortality gap. But is this association entirely mediated by differences in the socioeconomic composition of the black and white populations? Or does the racial opportunity gap have explanatory power net of differences in SES levels?
Table 3 present results from OLS regression models estimating the relationship between the racial opportunity gap and the racial mortality gap for males using both total population weights (Models 1–3) and black male only weights (Models 4–6). The first column presents the bivariate association, corresponding to the fitted lines in Fig. 1. We then adjust for a vector of covariates capturing within-sex, racial differences in economic outcomes that are commonly used in analyses of racial health disparities: unemployment, poverty, median income, and proportion with at least a four-year college degree. The coefficient on the racial opportunity gap remains substantively large and statistically significant after inclusion of these covariates and regardless of weighting schema: the point estimates in Models 2 and 4 indicate a one-point increase in the racial opportunity gap is associated with an increase of the racial mortality gap of about 6 deaths per 100,000 for males.
Table 3.
OLS models estimating association between racial opportunity gap and racial mortality gap, males.
| Dependent Variable: | Total Population Weights | Black Population Weights | ||||
|---|---|---|---|---|---|---|
| Male Racial Mortality Gap | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 |
| Opportunity Gap (W–B) | 16.320*** | 6.651** | 5.037* | 19.948*** | 6.189** | 7.474*** |
| (2.212) | (2.029) | (2.145) | (3.057) | (2.362) | (1.678) | |
| Unemployment Gap (B–W) | 5.721*** | 3.458** | 4.526*** | 2.213** | ||
| (1.445) | (1.333) | (1.104) | (0.796) | |||
| Poverty Gap (B–W) | 2.961*** | 3.662*** | 5.597*** | 5.398*** | ||
| (0.748) | (0.677) | (0.605) | (0.529) | |||
| Median Income Gap (W–B) | 0.246 | 0.862 | 1.419 | 0.889 | ||
| (0.807) | (0.837) | (0.796) | (0.809) | |||
| B.A. or Greater Gap (W–B) | 4.838*** | 4.755*** | 5.340*** | 5.429*** | ||
| (0.764) | (0.646) | (0.871) | (0.550) | |||
| State Fixed Effects | No | No | Yes | No | No | Yes |
| N | 1535 | 1535 | 1535 | 1535 | 1535 | 1535 |
| R-Square | 0.096 | 0.229 | 0.379 | 0.149 | 0.443 | 0.603 |
Notes: Data for racial mortality gaps, opportunity gaps, and economic gaps are pooled over 5 years (2013–2017). Robust standard errors in parentheses; *p < 0.05, **p < 0.01, ***p < 0.001. All models are weighted for county population.
The final model adds state fixed effects, an essential robustness check given the central role of states in shaping policies and institutions that influence both opportunity and mortality (Montez, Hayward, & Anna, 2019). Here again the estimated coefficient on the racial opportunity gap remains substantively large and statistically significant; even within states, counties with a larger racial opportunity gap also have a larger racial mortality gap for males, net of socioeconomic differences between the two groups.
Table 4 presents the corresponding set of models for females and reveals a similar pattern. The racial opportunity gap is positively correlated with the size of racial mortality gap across U.S. counties both before and after adjusting for differences in the socioeconomic status of the two groups. Notably, the point estimates for females are similar to those for males. Adding state fixed effects to our model reduces the estimated effect size in models using total population weights but not in models weighting by the size of the black female population.
Table 4.
OLS models estimating association between racial opportunity gap and racial mortality gap, females.
| Dependent Variable: | Total Population Weights | Black Population Weights | ||||
|---|---|---|---|---|---|---|
| Female Racial Mortality Gap | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 |
| Opportunity Gap (W–B) | 9.199*** | 6.536*** | 4.103 | 13.030*** | 8.097*** | 8.841*** |
| (1.831) | (1.911) | (2.587) | (1.544) | (1.767) | (1.341) | |
| Unemployment Gap (B–W) | −0.480 | −2.143 | 1.988* | −0.288 | ||
| (1.445) | (1.351) | (0.949) | (0.826) | |||
| Poverty Gap (B–W) | 2.664*** | 2.535** | 2.561*** | 2.283*** | ||
| (0.789) | (0.847) | (0.462) | (0.347) | |||
| Median Income Gap (W–B) | −0.184 | 0.713 | 0.089 | 0.452 | ||
| (1.401) | (1.415) | (1.194) | (1.254) | |||
| B.A. or Greater Gap (W–B) | 1.553* | 1.893** | 2.761*** | 2.597*** | ||
| (0.703) | (0.701) | (0.726) | (0.515) | |||
| State Fixed Effects | No | No | Yes | No | No | Yes |
| N | 1519 | 1519 | 1519 | 1519 | 1519 | 1519 |
| R-Square | 0.046 | 0.102 | 0.223 | 0.194 | 0.386 | 0.535 |
Discussion & conclusion
The analyses above demonstrate an association between the racial opportunity gap and racial mortality gap across U.S. counties. Notably, this association holds even after accounting for compositional differences in the socioeconomic status of blacks and whites, specifically poverty, unemployment, education and income, as well as differences in state policy environments. As a measure of structural racism, the opportunity gap offers an empirical and analytic framework for modeling the ‘underlying’—and often obscured—effect of place in generating racial disparities in SES and health outcomes.
How to understand exactly what aspects of place the racial opportunity gap is capturing? The answers—be it differential school quality, housing patterns, criminal justice policy, etc.—will likely vary considerably across localities. The opportunity gap can be thought of as a broad measure that aggregates up and sums across the varied specific features of place that have already been identified as generating racial health disparities. Immediate future work should examine how specific racialized features of place identified in other studies—such as residential segregation, education, incarceration or policy context—serves to mediate this association. We hasten to add, however, that the opportunity gap measure is a retrospective measure of place, as it is constructed based on the mobility outcomes for cohorts born in the early 1980s. Nevertheless, we think this specific measure—and the broader approach of using mobility data to operationalize opportunity structures—has substantial potential for population health research (O’Brien, Venkataramani, & Tsai, 2017).
The opportunity gap framework suggests that research delineating policies, institutions and other factors associated with upward economic mobility will by extension generate new insights into the structural determinants of racial health disparities. Such work is already underway, with recent papers documenting the role of education and labor markets (e.g. Rothstein, 2019), crime (Sharkey & Torrats-Espinosa, 2017), pollution (Manduca & Sampson, 2019; O'Brien et al., 2018), and history (Berger, 2018) in accounting for place-based differences in economic opportunity. More broadly, ongoing efforts to account for recent trends in mortality may find the opportunity gap framework useful when examining spatial patterns in the rise of ‘deaths of despair’ resulting from suicide, accidents, or drugs and alcohol (Woolf et al., 2018).
Moreover, pairing the racial opportunity gap with other pioneering efforts to measure place-based racism—be it through structural, cultural or interactive channels—may provide analytic leverage for disentangling and detailing the complex ways race interacts with place to shape health disparities. The measure may also prove useful in efforts to measure and identify how structural racism restricts flexible resources beyond SES that are important to health, such as prestige and power (Phelan & Link, 2015; Williams & Sternthal, 2010). An immediate next step is to identify whether and to what extent spatial variation in the racial opportunity gap maps on to differences in the lived experience and subjective perceptions of racism and discrimination experienced by African Americans.
The racial opportunity gap has important limitations. First, the measure captures the economic mobility experience of only one recent cohort; although the persistence of place-based inequalities have been widely documented, measuring the racial opportunity gap through time has clear empirical advantages. Second, by conditioning only on income, the racial opportunity gap measure does not account for the powerful role of wealth in structuring differences across groups. Third, although an effective summary measure of the effect of place in generating racial differences in life chances, the relative contribution of schools, the environment, policy context, and other local features of place in generating the racial opportunity gap remains opaque.
Critically, the most profound limitation of the racial opportunity gap is that it fails to adequately capture the myriad complex ways racism undermines human potential and shortens lives. Such a reality only underscores the need for population health researchers to continue to develop new frameworks to conceptualize, measure and model racism in empirical research on racial health disparities.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Rourke O'Brien: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing. Tiffany Neman: Conceptualization, Methodology, Formal analysis. Nathan Seltzer: Conceptualization, Methodology, Formal analysis. Linnea Evans: Conceptualization, Writing - original draft, Writing - review & editing. Atheendar Venkataramani: Conceptualization, Methodology, Writing - review & editing.
Declaration of competing interest
None.
Acknowledgement
This work was supported by a core grant to the Center for Demography and Ecology at the University of Wisconsin–Madison (P2C HD047873).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100564.
Notes: Data for racial mortality gaps, opportunity gaps, and economic gaps are pooled over 5 years (2013–2017). Robust standard errors in parentheses; *p < 0.05, **p < 0.01, ***p < 0.001. All models are weighted for county population.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Bailey Z., Krieger N., Agénor M., Graves J., Bassett M.T. Structural racism and health inequities in the USA: Evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Bauer G.R. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science & Medicine. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- Berger T. Places of persistence: Slavery and the geography of intergenerational mobility in the United States. Demography. 2018;55(4):1547–1565. doi: 10.1007/s13524-018-0693-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J., Venkataramani A.S., Williams D.R., Tsai A.C. Police killings and their spillover effects on the mental health of black Americans: A population-based, quasi-experimental study. The Lancet. 2018;392:302–310. doi: 10.1016/S0140-6736(18)31130-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning C.R., Cagney K.A., Ming W. Explaining variation in health status across space and time: Implications for racial and ethnic disparities in self-rated health. Social Science & Medicine. 2003;57(7):1221–1235. doi: 10.1016/s0277-9536(02)00502-6. [DOI] [PubMed] [Google Scholar]
- Brown T.H., Richardson L.J., Hargrove T.W., Thomas C.S. Using multiple-hierarchy stratification and life course approaches to understand health inequalities: The intersecting consequences of race, gender, SES, and age. Journal of Health and Social Behavior. 2016;57(2):200–222. doi: 10.1177/0022146516645165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmichael S., Hamilton C.V. Vintage Books; New York: 1967. Black Power: The politics of liberation in America. [Google Scholar]
- Chambers B.D., Erausquin J.T., Tanner A.E., Nichols T.R., Brown-Jeffy S. Testing the association between traditional and novel indicators of county-level structural racism and birth outcomes among black and white women. Journal of Racial and Ethnic Health Disparities. 2018;5(5):966–977. doi: 10.1007/s40615-017-0444-z. [DOI] [PubMed] [Google Scholar]
- Chetty R., Hendren N., Jones M.R., Porter S.R. National Bureau of Economic Research; 2018. Race and economic opportunity in the United States: An intergenerational perspective. Working Paper No. w24441. [Google Scholar]
- Crimmins E.M., Shim H., Zhang Y.S., Kim J.K. Differences between men and women in mortality and the health dimensions of the morbidity process. Clinical Chemistry. 2019;65(1):135–145. doi: 10.1373/clinchem.2018.288332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen M.R., Cummins C., Fuchs V.R. Geographic and racial variation in premature mortality in the US: Analyzing the disparities. PloS One. 2012;7(4) doi: 10.1371/journal.pone.0032930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham T.J., Croft J.B., Liu Y., Lu H., Eke P.I., Giles W.H. Vital signs: Racial disparities in age-specific mortality among blacks or African Americans — United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2017;66:444–456. doi: 10.15585/mmwr.mm6617e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebreab S.Y., Diez Roux A.V. Exploring racial disparities in CHD mortality between blacks and whites across the United States: A geographically weighted regression approach. Health & Place. 2012;18(5):1006–1014. doi: 10.1016/j.healthplace.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Ford C.L. Structural racism and health inequities: Old issues, new directions. Du Bois Review. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geruso M. Black-white disparities in life expectancy: How much can the standard SES variables explain? Demography. 2012;49(2):553–574. doi: 10.1007/s13524-011-0089-1. [DOI] [PubMed] [Google Scholar]
- Hardeman R.R., Medina E.M., Kozhimannil K.B. Structural racism and supporting black lives-the role of health professionals. New England Journal of Medicine. 2016;375(22):2113–2115. doi: 10.1056/NEJMp1609535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardeman R.R., Murphy K.A., Karbeah J'Mag, Backes Kozhimannil K. Naming institutionalized racism in the public health literature: A systematic literature review. Public Health Reports. 2018;133(3):240–249. doi: 10.1177/0033354918760574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer R.A. Black-white differences in health and mortality: A review and conceptual model. The Sociological Quarterly. 1996;37(1):105–125. [Google Scholar]
- Kershaw K.N., Diez Roux A.V., Burgard S.A., Lisabeth L.D., Mujahid M.S., Schulz A.J. Metropolitan-level racial residential segregation and black-white disparities in hypertension. American Journal of Epidemiology. 2011:1–9. doi: 10.1093/aje/kwr116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Methods for the scientific study of discrimination and health: An ecosocial approach. American Journal of Public Health. 2012;102(5):936–945. doi: 10.2105/AJPH.2011.300544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrine H., Klonoff E.A. The schedule of racist events: A measure of discrimination and a study of its negative physical and mental health consequences. Journal of Black Psychology. 1996;22(2):144–168. [Google Scholar]
- Lewis T.T., Cogburn C.D., Williams D.R. Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology. 2015;11:407–440. doi: 10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Life Expectancy National Center for Health Statistics 2018. https://www.cdc.gov/nchs/fastats/life-expectancy.htm Accessed May 2019.
- Lukachko A., Hatzenbuehler M.L., Keyes K.M. Structural racism and myocardial infarction in the United States. Social Science & Medicine. 2014;103:42–50. doi: 10.1016/j.socscimed.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manduca R., Sampson R.J. Punishing and toxic neighborhood environments independently predict the intergenerational social mobility of black and white children. Proceedings of the National Academy of Sciences. 2019;116(16):7772–7777. doi: 10.1073/pnas.1820464116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeilly M.D., Anderson N.B., Armstead C.A., Clark R., Corbett M., Robinson E.L. Perceived racism scale: A multidimensional assessment of the experience of white racism among African Americans. Ethnicity & Disease. 1996;6:154–166. [PubMed] [Google Scholar]
- Mendez D.D., Hogan V.K., Culhane J. Institutional racism and pregnancy health: Using Home Mortgage Disclosure act data to develop an index for mortgage discrimination at the community level. Public Health Reports. 2011;126(3):102–114. doi: 10.1177/00333549111260S315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez J.K., Hayward M.D., Anna Z. Educational disparities in adult health: U.S. States as institutional actors on the association. Socius. 2019 doi: 10.1177/2378023119835345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosrati E., Ash M., Marmot M., McKee M., Lawrence P., King The association between income and life expectancy revisited: Deindustrialization, incarceration and the widening health gap. International Journal of Epidemiology. 2017;47(3):720–730. doi: 10.1093/ije/dyx243. [DOI] [PubMed] [Google Scholar]
- Nuru-Jeter A.M., Michaels E.K., Thomas M.D., Reeves A.N., Thorpe R.J., Jr., LaVeist T.A. Relative roles of race versus socioeconomic position in studies of health inequalities: A matter of interpretation. Annual Review of Public Health. 2018;39:169–188. doi: 10.1146/annurev-publhealth-040617-014230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien, Rourke L., Neman T., Rudolph K., Casey J., Venkataramani A. Prenatal exposure to air pollution and intergenerational economic mobility: Evidence from US county birth cohorts. Social Science & Medicine. 2018;217:92–96. doi: 10.1016/j.socscimed.2018.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien R.L., Venkataramani A.S., Tsai A.C. Economic mobility and the mortality crisis among US middle-aged whites. Epidemiology. 2017;28.2:e12. doi: 10.1097/EDE.0000000000000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annual Review of Sociology. 2015;41:311–330. [Google Scholar]
- Richardson L.J., Brown T.H. (En) gendering racial disparities in health trajectories: A life course and intersectional analysis. SSM-Population Health. 2016;2:425–435. doi: 10.1016/j.ssmph.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein J. Inequality of educational opportunity? Schools as mediators of the intergenerational transmission of income. Journal of Labor Economics. 2019;37(S1):S85–S123. [Google Scholar]
- Sewell A.A. The racism-race reification process: A mesolevel political economic framework for understanding racial health disparities. Sociology of Race and Ethnicity. 2016;2(4):402–432. [Google Scholar]
- Sharkey P., Torrats-Espinosa G. The effect of violent crime on economic mobility. Journal of Urban Economics. 2017;102:22–33. [Google Scholar]
- Wildeman C., Wang E.A. Mass incarceration, public health, and widening inequality in the USA. The Lancet. 2017;389:10077. doi: 10.1016/S0140-6736(17)30259-3. 1464-1474. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Collins C. US socioeconomic and racial differences in health: Patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams D.R., Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. Sep-Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., González H.M., Williams S., Mohammed S.A., Moomal H., Stein D.J. Perceived discrimination, race and health in South Africa: Findings from the South Africa stress and health study. Social Science & Medicine. 2008;67:441–452. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A. Racism and health I: Pathways and scientific evidence. American Behavioral Scientist. 2013;57(8):1152–1173. doi: 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Sternthal M. Understanding racial-ethnic disparities in health: Sociological contributions. Journal of Health and Social Behavior. 2010;51(1_suppl):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Yan Yu J.S.J., Anderson N.B. Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Woolf S.H., Chapman D.A., Buchanich J.M., Bobby K.J., Zimmerman E.B., Blackburn S.M. Changes in midlife death rates across racial and ethnic groups in the United States: Systematic analysis of vital statistics. British Medical Journal. 2018;362 doi: 10.1136/bmj.k3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.