Over the past decade, 2 powerful scientific movements in the United States, population genetics and health disparities research, have re-ignited a contentious debate on the complex relationships between genes, race, and disease.1–3 The debate is fueled by the Human Genome Project, the increased technological capacity to map the entire human genome (the library of DNA building blocks), and the concerted national efforts to reduce racial disparities in health and health care.
Many scientists believe that an understanding of the unique patterns of genes across patient populations defined by race will help identify populations at risk of developing particular diseases and ultimately enable the medical profession to tailor preventive medicine and therapies to those most likely to respond.4 A central premise of this field of investigation is that race is an inherent biological characteristic that accurately reflects human ancestry and the flow of common threads of genetic material in biologically distinct populations over time and geography.
Health disparities research focuses on understanding the complex associations between race, health, and health care. Stimulated by the Healthy People 2010 initiative5 and an Institute of Medicine report documenting inequities in medical treatment among racial minorities,6 many health services, social sciences, and public health investigators have come to view race as a social and cultural construct, not a biological construct to be used in studies of race and human illness.
Differences of opinion on the appropriate way to apply the construct of race in biomedical and health services research raise 3 important questions for medical and public health practitioners, scientists, policymakers, and funding agencies committed to advancing both biomedical and health disparities research agendas: What are the arguments for and against using a biological definition of race in medical research? What is the best way to articulate a comprehensive health disparities research agenda? What are the current and future roles of genetics in advancing the health disparities research agenda?
USING A BIOLOGICAL DEFINITION OF RACE IN MEDICAL RESEARCH: PROS AND CONS
Scientists in the medical and public health research community are deeply divided about the associations between genes and race in determining the susceptibility, prevalence, and outcomes of human disease.1–3,7,8 Both sides use available genetic data and ethical arguments of social justice to support their arguments.
Pros
Recent population genetics studies have revealed large genetic variations across the 5 racial subpopulations that map to continental ancestry; researchers have found delineation of genetic clusters by racial group and race specificity of rare genetic variants.9–12 Those in favor of using a biological definition of race in medical science claim that these findings indicate that the frequency of variant alleles and the frequency of phenotypes (i.e., external expressions of genetic makeup) vary substantially by racial group, leading to racial differences in the expression of the phenotypes themselves in health and disease.1
This argument is bolstered by examples of rare Mendelian disorders for which the relationship of genes to race is readily apparent, for example, in the Amish, Ashkenazi Jewish, and French Canadian populations.1 Although genetic associations are more difficult to identify in complex genetic disorders, genetic variation by race has also been identified for Crohn’s disease and factor V Leiden, a genetic variant associated with thromboembolic disease.13–15 Proponents of a biological definition of race further argue that there may be important interactions between race and genetic characteristics in the susceptibility to disease, making such racial classification useful even when a genetic determinant of a complex disease is present in all racial groups.1 Currently, the strongest argument in favor of using a biological definition of race in medical science is the genomics movement, a field of scientific investigation that has recently gained momentum by promising to tailor medical therapies using race as a proxy for individual genotyping.4
There are a variety of more hypothetical scientific, social, and moral arguments in favor of using a biological definition of race.1,7 Proponents believe racial categories are useful in generating hypotheses about genetic and environmental risk factors for disease and argue that failure to include variables such as race will retard the progression of medical research. They posit that evaluating genetic differences that underlie health disparities is particularly appropriate when important racial differences persist after access to care and socioeconomic status are taken into account. Ignoring the role of genes in studies of racial differences in the causes, prevalence, and outcomes of diseases, they say, will not make such disparities disappear and will be detrimental to the very populations that opponents of using a biological definition of race seek to protect.
Cons
Those who argue against using a biological definition of race in medical science dispute the veracity of data obtained by researchers who claim to have identified a biological role for race in elucidating racial differences in the causes, prevalence, and outcomes of disease.3,16 The argument against begins with the premise that the species Homo sapiens consists of a single population and that biologically distinct human races do not exist. This premise is supported by genetic studies demonstrating that human beings share 99.9% of their DNA in common and the vast majority of genetic variation (90%–95%) occurs within, not across, human populations.16,17 Although opponents of a biological definition of race acknowledge that it is possible to classify geographically defined populations on the basis of clusters of genetic building blocks, they argue that the public health implications of such ancestral clustering of genes is controversial and that race at the ancestral or continental level has not been proven useful in terms of predicting individual diagnoses or individuals’ responses to drugs or causes of disease.3
These scientists argue that race is not useful for distinguishing polygenic phenotypes such as height, let alone complex diseases where there is little evidence that specific susceptibility-gene variants occur more frequently in different populations. Evidence that genes, not to mention relevant combinations of gene variants, substantially influence susceptibility to complex disease is very limited, making it impossible to predict the risk or outcomes of common disease on the basis of genotype. Opponents of the use of a biological definition of race believe that the immediate benefits of genomics are greatly overstated because it is impossible for race to provide the sensitivity and specificity needed to characterize DNA sequence variation for the purpose of guiding preventive or therapeutic medicine.
This camp also makes ethical and social justice arguments against the use of a biological definition of race in medical research.3,16,17 They use historical arguments to suggest that associating race, genes, and disease could result in unwarranted discrimination at the individual level and could, at worst, result in stigmatization of whole communities and even population eugenics. They argue that an unintended consequence of genetic reductionism, or categorizing biological risk by race, might be the exclusion of other, more relevant, social or environmental factors as potential explanations for the expression of health or disease. Similarly, they say, the promotion of specific drug therapies for a race-specific niche market could distract physicians from prescribing proven therapies. These scholars view the term “race” as a sociocultural construct that reflects an amalgamation of ancestry, education, language, literacy, and economic and social status.
ARTICULATING A HEALTH DISPARITIES RESEARCH AGENDA
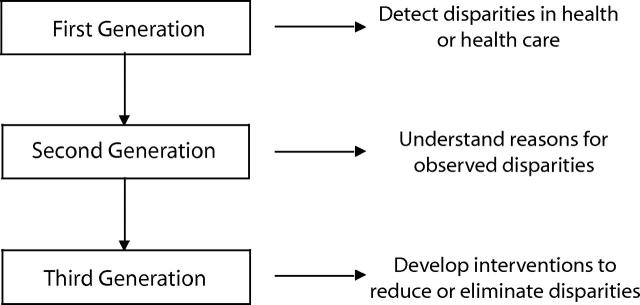
In an effort to meet the ambitious goals set forth in Healthy People 2010, investigators at the Center for Health Equity Research and Promotion (CHERP), a VA Center of Excellence whose mission is to detect, understand, and eliminate health disparities among vulnerable populations such as racial minorities,18 have articulated a health disparities research framework based in part on previous models of health disparities research19–21 (also A. M. Kilbourne et al., unpublished data, 2005). According to this framework (Figure 1 ▶), research in this field naturally progresses through 3 sequential phases or generations: from detecting disparities (first generation) to understanding their root causes (second generation) to devising interventions to reduce and eliminate disparities in health and health care (third generation). In framing the growing body of second-generation health disparities research, this model captures the complex set of individual, medical care provider, health care system, and broader social and environmental factors that could give rise to disparities in health and health care.
FIGURE 1—
The Center for Health Equity Research and Promotion framework for advancing health disparities research.
This framework also provides some insights into the relationships between disparities in health and disparities in health care. Although disparities in access to or delivery of health care services can cause or exacerbate disparities in health status, health status disparities may arise from individual, social, and environmental factors independent of any interactions with medical providers or the health care system. The model also suggests that interventions to reduce and eliminate health disparities (third-generation research) have multiple potential levers, ranging from individual knowledge and attitudes to provider behavior and communication to the organization and financing of the health care system to broader issues dealing with environmental safety and exposures.
Currently, the CHERP framework for health disparities research and the conceptual model held by many health services, social sciences, and public health researchers define race as a sociocultural construct rather than a set of predictable biological or genetic characteristics. This definition of race is based on a dearth of convincing scientific evidence for (1) a genetic basis for race, (2) a genetic explanation of observed racial disparities in the prevalence or outcomes of complex disease, and (3) the efficacy of race-based genomics to reduce or eliminate such disparities. It is further supported by an appreciation of the potentially negative individual and societal consequences of adopting a biological definition of race as described earlier.
THE ROLE OF GENETICS IN ADVANCING THE HEALTH DISPARITIES RESEARCH AGENDA
The ongoing debate over the application of race in medical research gives rise to important questions about the role of genetics in advancing the health disparities research agenda. What is the role of genetics in the detection of disparities (first-generation research)? In research to elucidate the root causes of disparities (second-generation research), do genes represent a new dimension of the individual that contributes to observed health disparities independently, or as part of an interaction with social or environmental factors? What is the role of genomics in eliminating health disparities (third-generation research)?
Genes appear to have no role in existing first-generation health disparities research, which typically relies on self-reported race (defined according to US Census Bureau categories) as collected in retrospective or prospective cohort studies or from administrative databases. Second-generation health disparities research has identified numerous patient, provider, health care system, and environmental factors that are independent of human biology as contributors to health disparities among racial minorities. Few would argue that lack of access to the health care system, poor nutritional status, biased treatment by health care providers, and unsafe living conditions are genetically determined, and few would argue that these factors are unlikely to play a role in health disparities.
The third generation of health disparities research is in the conception phase; to our knowledge, there are no published reports of interventions specifically designed to reduce or eliminate health disparities. Despite the Food and Drug Administration’s approval of race-specific pharmacotherapy to treat heart failure and glaucoma in African Americans,17,22 the jury is still out regarding the use of race to individualize medical therapies as a means of reducing health disparities.
Genetics and genomics do have the potential to advance the health disparities research agenda in the future. Given the historically polarized debate over the role of race in medical studies, the heretofore unproven role of genetics in disparities research, and the secular nature of scientific investigation, a new research paradigm is needed to move the intersecting fields of genetics and health disparities research forward. The National Institutes of Health’s road map of inter- and multidisciplinary research represents an effective prescription for change.23
As the fields of genetics and health disparities research mature, scholars from all disciplines involved in the effort to eliminate health disparities must fully engage in the ongoing scientific, ethical, and moral dialogue on the relationship between genes, race, and disease. In addition, collaboration between investigators in these 2 fields is essential to gaining a better understanding of the origins of health disparities, determining the contributory role of genes, and identifying the most effective interventions to eliminate disparities. The US Department of Energy and Howard University’s recent sponsorship of a conference on these topics is promising, as is the National Institutes of Health’s support of the National Human Genome Research Institute and interdisciplinary research centers of excellence.24,25 As researchers committed to the attainment of health equity, we are cautiously optimistic that focused multidisciplinary research and educational efforts such as these will inform the collective scientific wisdom on the future role of genetics in advancing the health disparities research agenda.
Acknowledgments
Michael J. Fine is supported in part by a K24 Mid-Career Development Award from the National Institute of Allergy and Infectious Diseases (award 5K24AI001769-05). Said A. Ibrahim is the recipient of an Advanced Career Development Award from the VA Health Services Research and Development Service and the Harold Amos Faculty Development Award from the Robert Wood Johnson Foundation (award 47429-MFD). Stephen B. Thomas receives support from the National Center for Minority Health and Health Disparities’ Project EXPORT—Excellence in Partnerships for Community Outreach, Research on Health Disparities, and Training (grant 5P60 MD00207-04).
The authors would like to thank Mary B. Walsh for her critical comments and editorial assistance and Antoinette Klein for word processing.
Note.The views expressed in this editorial are those of the authors and do not represent those of the Department of Veterans Affairs.
References
- 1.Burchard E.G., Ziv E, Coyle N, et al. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med. 2003; 348:1170–1175. [DOI] [PubMed] [Google Scholar]
- 2.Phimister EG. Medicine and the racial divide. N Engl J Med. 2003;348: 1081–1082. [DOI] [PubMed] [Google Scholar]
- 3.Cooper RS, Kaufman JS, Ward R. Race and genomics. N Engl J Med. 2003;348:1166–1170. [DOI] [PubMed] [Google Scholar]
- 4.Citrin T, Modell S. Genomics and Public Health: Ethical, Legal, and Social Issues. Atlanta, Ga: Office of Genomics and Disease Prevention, Centers for Disease Control and Prevention; 2004.
- 5.Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Dept of Health and Human Services; November 2000.
- 6.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. [PubMed]
- 7.Livingston IL, ed. Praeger Handbook of Black American Health: Policies and Issues behind Disparities in Health. 2nd ed. Westport, Conn: Greenwood Publishing Group; 2004.
- 8.Shields AE, Fortun M, Hammonds EM, et al. The use of race variables in genetic studies of complex traits and the goal of reducing health disparities: a transdisciplinary perspective. Am Psychol. 2005;60:77–103. [DOI] [PubMed] [Google Scholar]
- 9.Mountain JL, Cavalli-Sforza LL. Multilocus genotypes, a tree of individuals, and human evolutionary history. Am J Hum Genet. 1997;61:705–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stephens JC, Schneider JA, Tanguay DA, et al. Haplotype variation and linkage disequilibrium in 313 human genes. Science. 2001;293:489–493. [DOI] [PubMed] [Google Scholar]
- 11.Wilson JF, Weale ME, Smith AC, et al. Population genetic structure of variable drug response. Nat Genet. 2001;29:265–269. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg NA, Pritchard JK, Weber JL, et al. Genetic structure of human populations. Science. 2002;298: 2381–2385. [DOI] [PubMed] [Google Scholar]
- 13.Ridker PM, Miletich JP, Hennekens CH, Buring JE. Ethnic distribution of factor V Leiden in 4047 men and women. Implications for venous thromboembolism screening. JAMA. 1997; 277:1305–1307. [PubMed] [Google Scholar]
- 14.Shen MC, Lin JS, Tsay W. High prevalence of antithrombin III, protein C and protein S deficiency, but no factor V Leiden mutation in venous thrombophilic Chinese patients in Taiwan. Thromb Res. 1997;87:377–385. [DOI] [PubMed] [Google Scholar]
- 15.Hugot JP, Chamaillard M, Zouali H, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature. 2001;411: 599–603. [DOI] [PubMed] [Google Scholar]
- 16.Braun L. Race, ethnicity, and health: can genetics explain disparities? Perspect Biol Med. 2002;45:159–174. [DOI] [PubMed] [Google Scholar]
- 17.Lee SS, Mountain J, Koenig BA. The meanings of “race” in the new genomics: implications for health disparities research. Yale J Health Policy Law Ethics. Spring 2001;1:33–75. [PubMed] [Google Scholar]
- 18.Center for Health Equity Research and Promotion. July 2005. Available at: http://www.cherp.org. Accessed July 27, 2005.
- 19.Braveman PA. Monitoring equity in health and healthcare: a conceptual framework. J Health Popul Nutr. Sep 2003;21(3):181–192. [PubMed] [Google Scholar]
- 20.Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. J Gen Intern Med. Jun 2002;17(6):477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rathore SS, Krumholz HM. Differences, disparities, and biases: clarifying racial variations in health care use. Ann Intern Med. Oct 19 2004;141(8): 635–638. [DOI] [PubMed] [Google Scholar]
- 22.Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351(20): 2049–2057. [DOI] [PubMed] [Google Scholar]
- 23.National Institutes of Health. NIH roadmap: accelerating medical discovery to improve health. Available at: http://nihroadmap.nih.gov. Accessed July 28, 2005.
- 24.Patrinos A. “Race” and the human genome. Nat Genet. 2004;36(11 suppl):S1–S2. [DOI] [PubMed] [Google Scholar]
- 25.The National Human Genome Research Institute. June, 2005. Available at: http://www.genome.gov. Accessed July 27, 2005.