Before her ancestry test, all Jessica Ewing knew about her father’s lineage was that she came from a family of Mexican migrant workers who moved wherever there was crop-picking work. “It’s hard to pinpoint where your family members come from if you’re poor, moving around a lot and lack education,” Ewing said. “It makes record-keeping impossible.”
She had wanted to do DNA testing for years, but kits like 23andMe, with their $100 price tag, were out of her already-stretched budget. Then Ewing learned about a free ancestry test from Spectrum Biobank, whose aim is to gather genetic data from communities often underrepresented in genetics research. She signed up online, received her testing kit immediately and got her results within a few weeks. She discovered Indigenous Mexican ancestry on her father’s side and Finnish and Scottish roots on her mother’s side that she didn’t know about. “I was shocked, to say the least,” Ewing said.
The win, she said, was twofold: Free DNA kits like Spectrum’s are helpful not only to people searching for their ancestry but also to advancing medicine.
“Most of these other biobanks are full of data, but what percentage of those are from people like me, or what percentage of clinical trials are done based on people like me?” said Ewing. “We are important, too.”
Non-European populations have historically been excluded from genetic studies and databases, like the National Human Genome Research Institute, and make up only 14% of genetic data. While popular DNA testing companies like 23andMe and Ancestry.com share their large data pools with academic, nonprofit and industry partners, they are self-selecting for users who can afford their tests. Even the future of the federal government’s initiatives to diversify genetic studies are uncertain with the Trump administration’s recent freeze of research funds.
All of this equates to underrepresented demographics being potentially excluded from scientific breakthroughs. For example, even though Native Americans have significantly higher rates of asthma, diabetes and cardiovascular disease, few studies have been conducted on Native-specific treatments.
Spectrum and the Native BioData Consortium are trying to fill these gaps. Around 80% of Spectrum’s test-takers are people of color, and the biobank is collaborating with the University of California San Francisco to track cardiovascular illnesses among South Asians. The Native Biodata Consortium is establishing a protocol for Native ownership of genetic data and has partnered with Stanford University to investigate Native-specific triggers for rheumatoid arthritis.
“Just the fact that our biobank is flipped — rather than having 80% or more white European data, we have the reverse of 80% non-European — that in itself is a powerful thing,” said Yambazi Banda, Spectrum’s executive director. “We have built trust with people to share their personal data despite the wrongs that have been done to minority groups over the years by institutions.”
Increasing representation in DNA data
Last year, a high-profile breach of 23andMe exposed weaknesses in genetic databases after hackers exploited the data leak of 7 million users to target people of Chinese and Ashkenazi Jewish descent. These communities, already facing threats and identity-based hate crimes, are now facing potential cybersecurity attacks.
The breach added to the negative attitudes vulnerable populations have toward storing and studying genetic data. The lack of people of color in genetic testing and clinical trials can be attributed to factors like distrust in the medical system after historically misusing data, lower numbers of NIH grants for researchers of color and cultural barriers. Without genetic information from specific communities, underrepresented populations may miss out on treatments or suffer life-threatening risks from medications that weren’t properly tested on them.
“It takes a lot of effort to build trust with communities and reach them in their own language,” UCSF medical school professor Alka Kanaya said. “Until now, there hasn’t been much community engagement by researchers to recruit diverse participants.”
To widen its genetic pool, Spectrum has been recruiting participants of color via social media and is building relationships with trusted organizations. While 23andMe filed for bankruptcy last month, leading to anxiety over additional user privacy violations, Spectrum said that all of their data is de-identified and users can see what their data is being used for and request deletion at any time.

When Kanaya needed help for a study, called MASALA, which looks at why South Asians seem to have a higher prevalence of heart disease, Spectrum stepped in to sequence genomes, or analyze a person’s entire genetic makeup. “Our combined goal was to use data to see if certain diseases show up more frequently in a group,” Kanaya said.
Prior to leading MASALA, she hadn’t come across a long-term study about heart disease in that community. “South Asians make up almost 25% of the world’s population, but in terms of genetic databases or biobanks, we only represent 2% of the data,” said Kanaya.
For the past decade, the National Institutes of Health’s All Of Us program has also been providing genetic data for studies like MASALA. But with the Trump administration’s cuts to NIH funding, Kanaya is waiting to see whether All Of Us and the MASALA funding will be renewed. “All this work that we’ve done may not reach fruition,” Kanaya said. “We may not see the data emerge.”
In the meantime, Spectrum will continue working to help sequence data from the study and recruit participants of color. Its goal is to send out 10,000 additional ancestry kits this year.
Protecting valuable genetic data from exploitation
According to Native BioData Consortium executive director Joseph Yracheta, science had neglected Native Americans for a long time because of their lack of market value.
“Before DNA testing, we were left out of scientific research because we don’t have private insurance and we’re too small of a population to make money for Big Pharma,” Yracheta said.
It’s only been in recent years that pharmaceutical companies have realized that Indigenous genetic data holds the potential for scientific breakthroughs. Beneficial gene variants are easier to identify in historically isolated groups like Indigenous communities and can spur drug development for the wider population. “We’re like the Rosetta Stone for everybody else,” said Yracheta. “We’re a huge asset to science.”
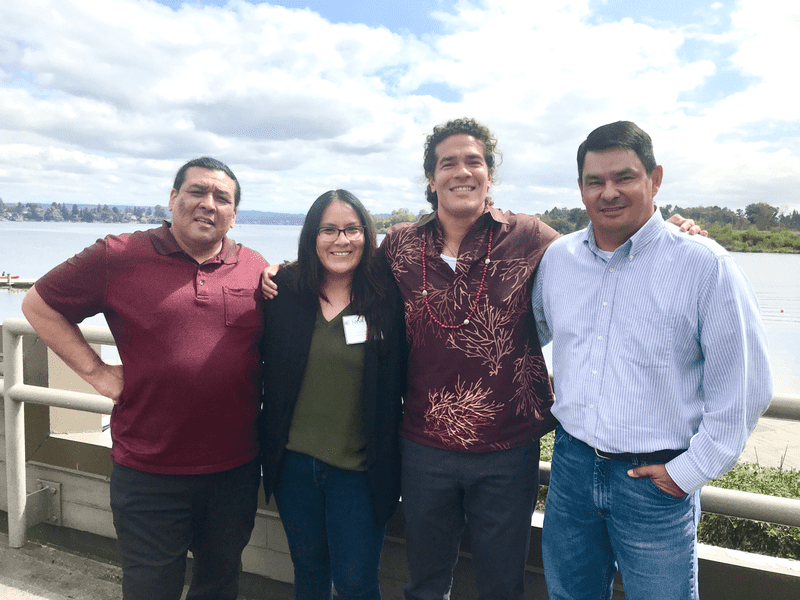
However, that value can lead to exploitation by research institutions. In 2004, Havasupai Tribe members sued Arizona State University for sharing their genetic samples for research outside of their consent. Then in 2019, U.S. researchers attempted to patent a clinical test after studying obesity in Samoans without sharing their findings with their Samoan collaborators. Meanwhile, many high-profit drugs, like those treating heart disease and cancer, are derived from Indigenous plant medicines by pharmaceutical companies that have often exploited natural resources.
“Right now, universities or research institutions are the holders and owners of genetic data and any patents that come out of the research,” Yracheta explained. “The way the rules are set up doesn’t give us any ownership or rights to our own data.”
To fix that, Stanford and the Native BioData Consortium received a $9 million grant from the NIH to establish new legal frameworks for public health data sharing. The consortium now facilitates data transfer ownership and usage agreements so tribes can control their own data. “If you’re not smart enough to protect your interests, these institutions will claim everything,” Yracheta said.
The accessibility and transparency of these biobanks have benefited participants like Ewing in ways she never imagined. “I believe it’s very important that everyone gets a chance to learn about their ancestry,” she said. “It’s influenced a lot of things — everything from the way I look at my preferences, even to the patterns I have in my day-to-day life.”